When you start taking an antipsychotic medication, your doctor focuses on stopping hallucinations or calming mood swings. But there’s another silent threat hiding in plain sight: your metabolism. Many people don’t realize that the very drugs helping them manage psychosis can also raise their risk of weight gain, diabetes, and heart disease-sometimes within weeks of starting treatment.
Why Antipsychotics Change Your Body’s Chemistry
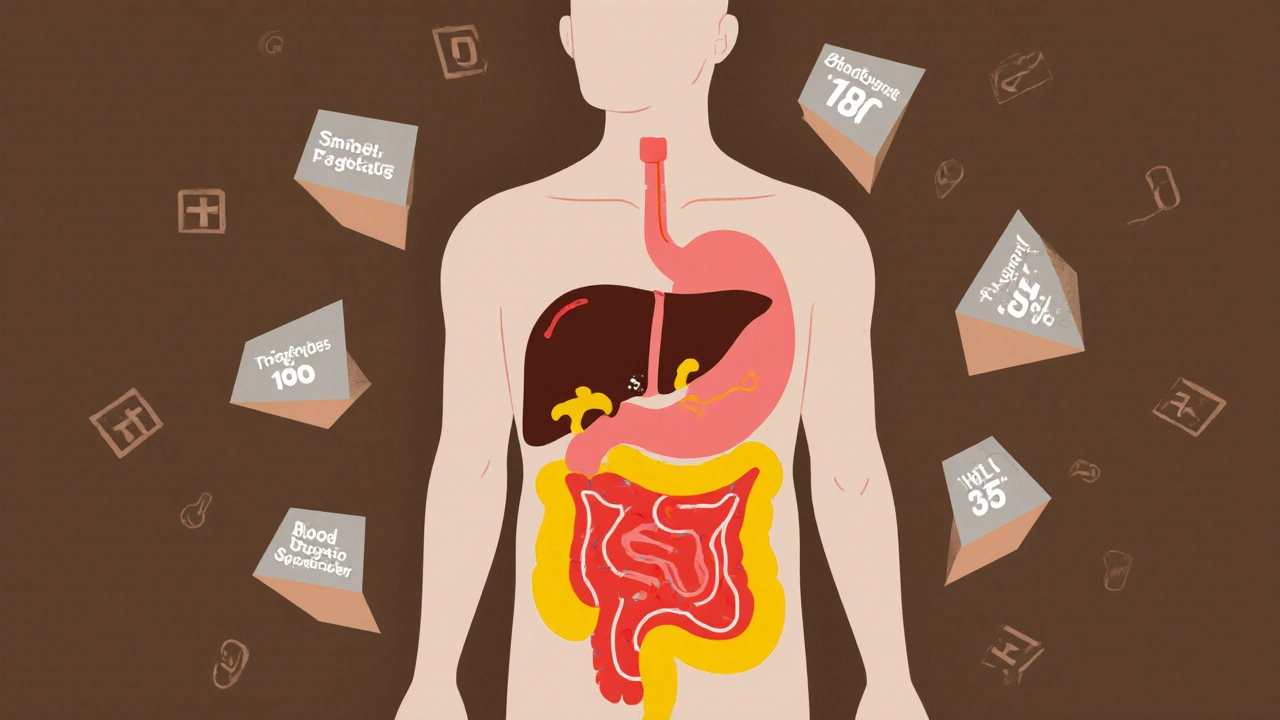
Second-generation antipsychotics (SGAs), like olanzapine, clozapine, and quetiapine, work differently than older drugs. They block dopamine and serotonin receptors in the brain to reduce psychotic symptoms. But those same receptors exist in your fat tissue, liver, pancreas, and muscles. When antipsychotics hit those spots, they mess with how your body handles sugar and fat.It’s not just about eating more. Even before you notice weight gain, your blood sugar can rise, your triglycerides climb, and your good cholesterol (HDL) drops. Research shows these changes can begin in the first few weeks of treatment-long before the scale moves. That’s why waiting to check your numbers until you’ve gained 10 pounds is too late.
Some drugs are worse than others. Olanzapine and clozapine carry the highest risk. In the CATIE study, people on olanzapine gained an average of 2 pounds per month. About 30% gained so much weight they had to stop the drug. On the other hand, ziprasidone, lurasidone, and aripiprazole are much gentler on your metabolism. If you’re starting treatment and have a family history of diabetes or heart disease, your doctor should consider these safer options first.
The Real Danger: Metabolic Syndrome
Metabolic syndrome isn’t one condition-it’s a cluster of five warning signs:- Waist circumference over 40 inches (men) or 35 inches (women)
- Triglycerides above 150 mg/dL
- HDL cholesterol below 40 mg/dL (men) or 50 mg/dL (women)
- Blood pressure at or above 130/85 mmHg
- Fasting blood sugar of 100 mg/dL or higher
If you have three or more of these, you have metabolic syndrome. And if you’re taking an antipsychotic, your chance of developing it jumps to between 32% and 68%. Compare that to just 3.3% to 26% in people not on these drugs. That’s a 3-fold increase in risk.
What does that mean for your future? Three times the chance of a heart attack. Three times the chance of a stroke. People with metabolic syndrome die younger-on average, 6.9 years sooner-mainly from heart disease. And this isn’t rare. One in three people on antipsychotics will develop this condition.
Who’s at Highest Risk?
It’s not just about the drug. Your genetics, lifestyle, and mental illness itself all play a role. People with schizophrenia already have a higher baseline risk for metabolic problems, even before taking medication. Add smoking, poor diet, and lack of exercise-and the numbers get worse.Young adults starting antipsychotics are especially vulnerable. Their bodies are still adjusting to hormonal changes, and weight gain hits harder. Studies show that up to 50% of patients stop taking their meds because of weight gain. That’s not laziness-it’s survival. When your body feels like it’s betraying you, staying on the drug becomes impossible.
And it’s not just oral pills. Long-acting injectables (LAI) don’t reduce metabolic risk. Whether you get your medication by mouth or shot, your body still reacts the same way. So if you’re on an LAI and your doctor isn’t checking your blood sugar or waistline, you’re being left unprotected.
What Needs to Be Checked-and When
There’s a clear, evidence-based plan for monitoring. Yet most patients never get it. A 2023 review found that nearly half of people on antipsychotics haven’t had their weight or blood pressure checked in over a year. That’s unacceptable.Here’s what your care team should do:
- Before starting: Measure weight, BMI, waist circumference, blood pressure, fasting glucose, and lipid panel (cholesterol and triglycerides).
- At 4 weeks: Check weight and blood pressure. If you’ve gained more than 5% of your body weight, investigate further.
- At 12 weeks: Repeat fasting glucose and lipid panel. This is when early signs of insulin resistance often show up.
- At 24 weeks: Full metabolic panel again. If everything’s stable, move to annual checks.
- Every 3-12 months after: Continue monitoring based on your risk level. High-risk patients (those on olanzapine, with obesity, or family history of diabetes) need checks every 3 months.
Don’t wait for symptoms. High blood sugar doesn’t cause pain. High cholesterol doesn’t make you tired. By the time you feel something, the damage may already be done.
What to Do If Your Numbers Go Up
If your tests show rising glucose, triglycerides, or waist size, you’re not stuck. There are real options.Option 1: Lifestyle changes
Simple, consistent habits make a difference. A structured diet and exercise program can cut weight gain in half. Walking 30 minutes a day, five days a week, improves insulin sensitivity. Cutting sugary drinks and processed carbs helps more than you think. You don’t need a gym membership-just movement.
Option 2: Medication adjustments
If you’re on olanzapine or clozapine and your metabolic markers are climbing, talk to your psychiatrist about switching. Yes, clozapine works wonders for treatment-resistant schizophrenia-but it doesn’t mean you have to accept diabetes as the price. Switching to aripiprazole or lurasidone can stabilize your weight and blood sugar without losing symptom control. Many patients do this successfully.
Option 3: Add a metabolic drug
Metformin, a common diabetes medication, has been shown in multiple studies to reduce antipsychotic-induced weight gain by up to 40%. It’s safe, cheap, and well-tolerated. Some clinics now prescribe it routinely to people starting SGAs. Ask your doctor if it’s right for you.

The Big Picture: Safety vs. Effectiveness
Antipsychotics save lives. They stop people from hearing voices that tell them to hurt themselves. They prevent manic episodes that lead to financial ruin or hospitalization. But if the treatment kills you faster than the illness, we’ve lost the point.Doctors are trained to treat psychosis. But metabolic health? That’s often an afterthought. The American Psychiatric Association, the American Diabetes Association, and the World Health Organization all agree: metabolic monitoring is non-negotiable. Yet in real-world clinics, it’s still the exception, not the rule.
If you’re on an antipsychotic, you need to be your own advocate. Bring a printout of the monitoring guidelines. Ask for your numbers. Push back if you’re told, “You’ll be fine.” Your body is not a gamble. The science is clear: early detection saves lives.
What You Can Do Today
You don’t have to wait for your next appointment.- Write down your weight and waist size now. Compare it in 30 days.
- Track your meals for a week. Are you drinking soda or juice? Eating fast food? That matters.
- Ask your doctor: “What’s my fasting glucose? My triglycerides? My HDL?”
- If you’re on olanzapine or clozapine and haven’t had a lipid panel in the last 6 months, request one.
- Find a dietitian who understands mental illness. They know how to help without triggering disordered eating.
Antipsychotics are powerful tools. But they’re not magic. They come with real, measurable risks-and those risks are preventable. The goal isn’t to avoid medication. It’s to use it safely. Your mind matters. So does your heart, your liver, and your future.

Andrew Forthmuller
So you're telling me my olanzapine is slowly turning me into a diabetic fat sack? Cool. Thanks for the heads up.