When you need a cheaper version of a brand-name pill, you probably reach for a generic. It’s the same active ingredient, same effect, same price cut. But what if your medicine isn’t a pill? What if it’s an injection for rheumatoid arthritis, cancer, or Crohn’s disease? That’s where biosimilars come in - the closest thing to generics for complex biologic drugs.
Why Biosimilars Aren’t Just Like Regular Generics
Regular generics are exact chemical copies of brand-name drugs like ibuprofen or metformin. They’re made from simple molecules, so manufacturers can replicate them perfectly. Biosimilars? They’re not copies. They’re highly similar versions of biologic drugs - proteins made from living cells, like antibodies or hormones. Think of it like trying to recreate a handmade quilt. Two quilts can look almost identical, but the stitching, thread, and texture will have tiny differences. That’s how biosimilars work. They’re not identical, but they’re close enough that they work the same way in your body. The FDA requires biosimilars to show no clinically meaningful difference in safety, purity, or effectiveness compared to the original biologic. That means if you’ve been taking Humira for psoriasis, switching to its biosimilar - say, Amjevita - won’t change how well your symptoms are controlled. But unlike generics, which go through a simpler approval process, biosimilars need years of testing: protein structure analysis, immune response studies, clinical trials in thousands of patients. It’s not just chemistry. It’s biology.Interchangeable Biosimilars: The Closest Thing to an Authorized Generic
There’s a special category within biosimilars called interchangeable. These are the ones that can be swapped at the pharmacy without asking your doctor - just like generics. In 2023, the FDA approved the first interchangeable biosimilar for Humira (adalimumab). That was a big deal. Before that, even if your insurance wanted you to switch, your doctor had to approve it. Now, in states with substitution laws, pharmacists can switch you automatically. But here’s the catch: only 32 out of 50 U.S. states have laws allowing this kind of substitution. In places like California, New York, and Texas, you might get switched without a second thought. In others, you’ll still need a new prescription. Insurance companies love interchangeable biosimilars because they cut costs faster. But patients? Some are nervous. A 2022 Arthritis Foundation survey found 37% of patients were forced to switch to a biosimilar by their insurer - and while only 12% had worse symptoms, the disruption alone caused stress, missed doses, and confusion.Cost Savings: Not as Big as You Might Think
Generics can save you 80-85% off brand-name prices. Biosimilars? They’re more like 10-50%. Why the smaller cut? Because making a biologic isn’t cheap. These drugs are grown in living cells - yeast, bacteria, or hamster ovary cells. The process is finicky. One batch might produce slightly different protein shapes than the next. That’s normal. But it means manufacturing is harder, slower, and more expensive than making a tablet. So even though biosimilars are cheaper, they’re not dirt cheap. Still, the savings add up. In 2023, biosimilars helped give over 344 million extra days of treatment to patients who otherwise couldn’t afford their medicine. For someone on a $1,200 monthly infusion for breast cancer, switching to a biosimilar dropped their cost to $450. That’s life-changing. Medicare Part D plans now cover 62% of biosimilars at the same tier as the original biologic. That means lower copays. More people are getting treated. More lives are being saved.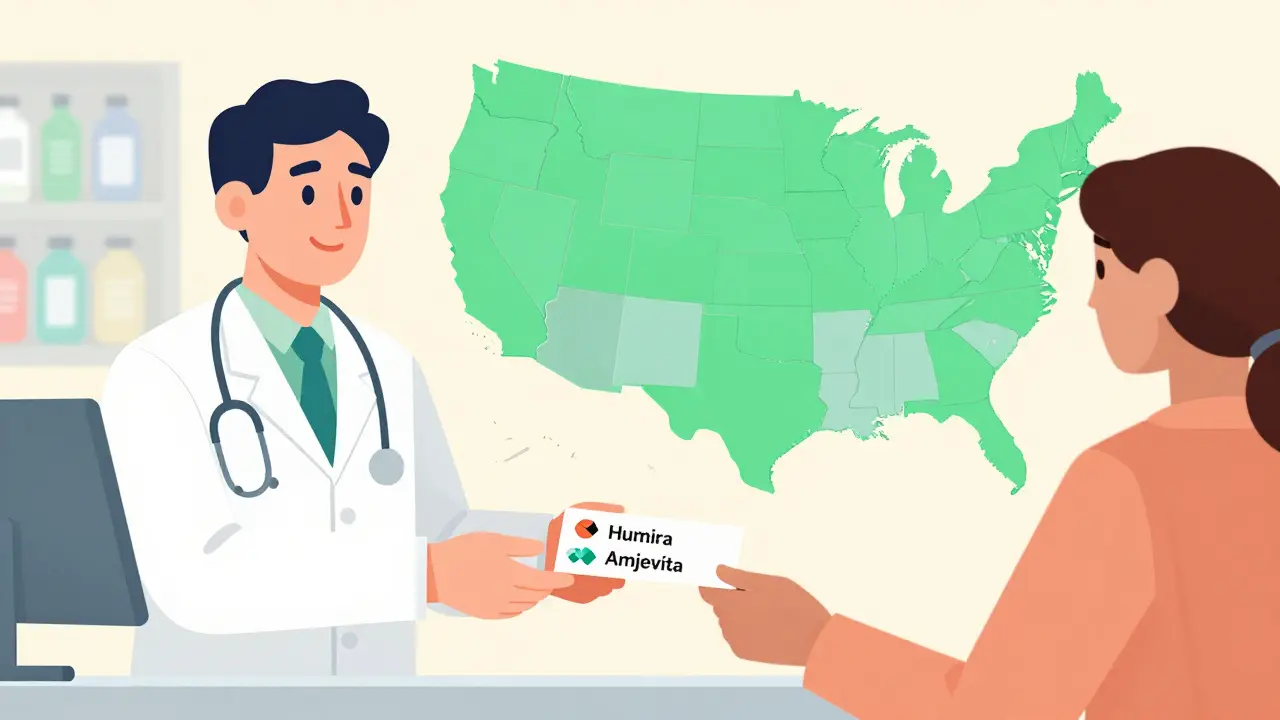
Why Aren’t More People Using Them?
You’d think with FDA approval, cost savings, and proven safety, biosimilars would be everywhere. But they’re not. Only about 18% of biologic prescriptions in the U.S. are filled with biosimilars. Why? First, confusion. Many patients and even some doctors think biosimilars are “less effective” or “experimental.” They’re not. The FDA says they’re as safe and effective as the original. Second, fear of switching. One Reddit user shared a story about a rheumatoid arthritis patient who got switched three times between the original drug and two different biosimilars - and started having injection site reactions. Was it the biosimilars? Unclear. But the fear stuck. Third, pharma companies fight hard to protect their market. They file dozens of patents, delay approvals, and pay hospitals not to switch. In 2023, the average biosimilar faced 14.7 patent challenges before even hitting the market.What’s Changing in 2026?
The tide is turning. The FDA approved 76 biosimilars by late 2023, and they’re targeting 15-20 new ones every year through 2025. Major biologics like Enbrel, Remicade, and Rituxan are losing patent protection soon. That means more biosimilars will flood the market. By 2028, $115 billion in global biologic sales will be open to competition. That’s not just savings - that’s access. Hospitals are leading the way. Eighty-seven percent now have formal biosimilar adoption policies. They’re saving millions. Medicare is expected to save $53 billion between 2024 and 2033. The Congressional Budget Office says biosimilars could cut U.S. healthcare spending by $314 billion over the next decade. And the science keeps getting better. The FDA updated its guidance in May 2023 to make it easier for companies to prove interchangeability. New labeling rules now require clear identification of the reference product, so patients know exactly what they’re getting.
What You Should Do If You’re on a Biologic
If you’re taking a biologic drug - whether it’s for arthritis, cancer, or an autoimmune disease - here’s what to do:- Ask your doctor: “Is there a biosimilar available for my medication?”
- Call your pharmacy: “Is my prescription being filled with a biosimilar?”
- Check your insurance formulary: Are biosimilars covered at the same cost-sharing level?
- Don’t panic if you’re switched. Track your symptoms. If you feel worse, tell your doctor immediately.
- Know your state’s laws. If you live in a state with substitution laws, your pharmacist can switch you without telling your doctor.
Bottom Line
Biosimilars aren’t generics. But they’re the best alternative we have for complex biologic drugs. They’re safe. They’re effective. And they’re getting cheaper, faster, and more available every year. The goal isn’t to replace the original - it’s to make life-saving treatments affordable for everyone. If you’re on a biologic, don’t assume you’re stuck paying full price. Ask questions. Know your options. And don’t let fear stop you from saving money - and maybe even saving your life.Are biosimilars as safe as the original biologic drugs?
Yes. The FDA requires biosimilars to show no clinically meaningful differences in safety, purity, or effectiveness compared to the original biologic. Thousands of patients have been studied in clinical trials, and real-world data from hospitals and clinics confirm they work the same way. Patients taking biosimilars don’t experience more side effects than those taking the brand-name version.
Can pharmacists automatically switch me to a biosimilar?
Only if your biosimilar is designated as “interchangeable” and your state allows pharmacist substitution. As of 2026, 32 U.S. states - including California, New York, and Texas - have laws permitting this. In other states, your doctor must approve the switch. Always check with your pharmacist and review your prescription label to confirm what you’re receiving.
Why are biosimilars cheaper but not as cheap as generics?
Biologics are made from living cells, not chemicals. Manufacturing them is complex, expensive, and requires strict controls to ensure consistency. Even small changes in temperature or cell culture can affect the final product. That means biosimilar manufacturers face higher production costs than generic pill makers, so savings are smaller - typically 10% to 50% instead of 80%+.
Do biosimilars cause more side effects?
No. Clinical trials and post-market monitoring show biosimilars have the same side effect profile as their reference products. Some patients report injection site reactions or flu-like symptoms after switching, but these are usually mild and temporary. In rare cases, repeated switching between multiple biosimilars has been linked to new reactions - but it’s unclear if that’s due to the drugs themselves or changes in manufacturing batches.
How do I know if I’m getting a biosimilar?
Check your prescription label or pharmacy receipt. Biosimilars have a different brand name than the original drug - for example, Amjevita instead of Humira. The FDA requires all biosimilars to clearly list the reference product on the label. You can also ask your pharmacist directly: “Is this a biosimilar?” They’re required to tell you.
Will my insurance force me to switch to a biosimilar?
Many insurers do, especially if the biosimilar is cheaper and covered at a lower tier. But you have rights. If your doctor says you need the original biologic for medical reasons, they can file an exception. Always ask your insurer for a copy of their formulary and check if your drug is listed as a preferred biosimilar. If you’re forced to switch and feel worse, contact your doctor right away.


Ashley Karanja
Okay, so let me just say this - biosimilars are basically the yoga instructors of the pharmaceutical world. They’re not the exact same as the original biologic, but they’re close enough to give you the same zen-like relief from inflammation without the $1,200 monthly price tag. I’ve been on Humira for 7 years, switched to Amjevita last year, and honestly? My psoriasis didn’t care. My wallet did. 🙌 The FDA’s standards aren’t just bureaucratic red tape - they’re a lifeline. Also, I love how the FDA now requires clear labeling. No more guessing games. We deserve transparency, not corporate obfuscation.