Most people who lose weight gain it back. Not because they lack willpower, but because they never fixed the thoughts that made them overeat in the first place. If you’ve ever thought, "One bite ruins everything," or "I’ll start again Monday," you’re not failing-you’re stuck in a mental loop most diets ignore. Behavioral weight loss therapy, specifically cognitive behavioral therapy (CBT), isn’t about counting calories or punishing yourself. It’s about rewiring the thoughts that drive overeating. And it works.
Why Diets Fail and CBT Succeeds
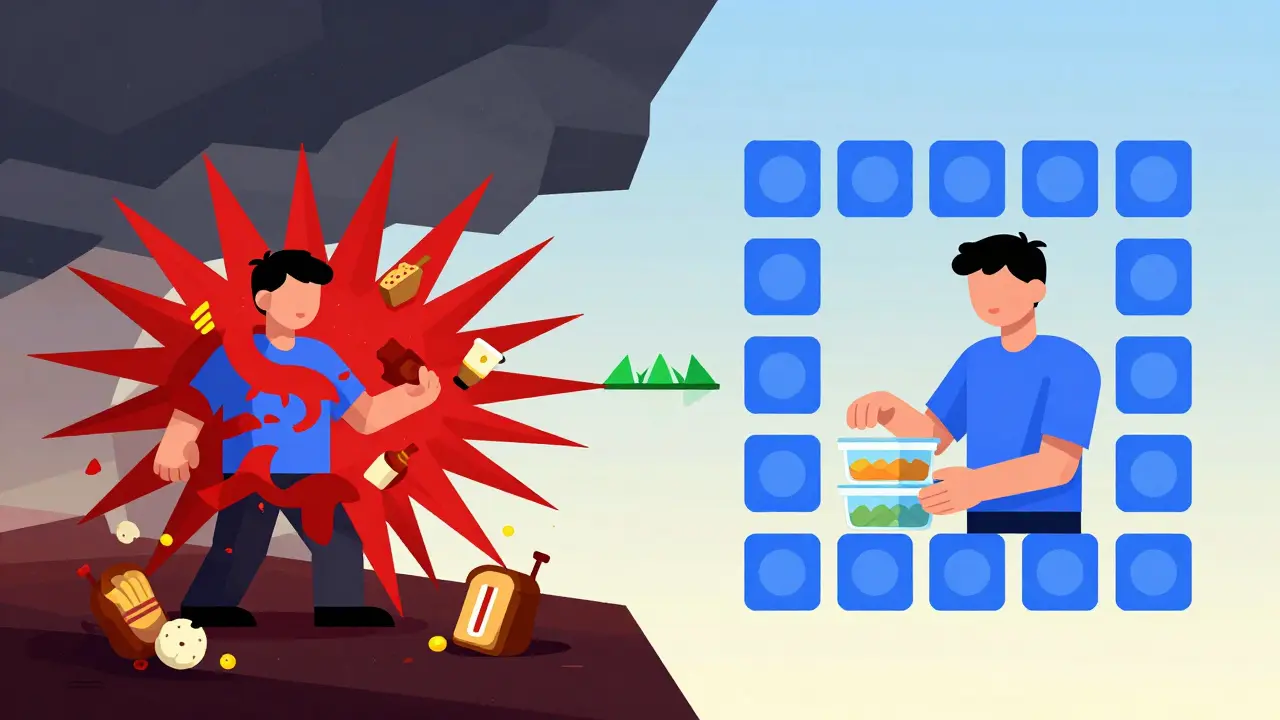
Diets that focus only on food and exercise treat weight like a math problem: eat less, move more. But your brain isn’t a calculator. It’s a survival machine. When you restrict food, your brain doesn’t see discipline-it sees famine. It triggers cravings, stress, and emotional eating to protect you. That’s why 80% of people who lose weight regain it within two years.
CBT flips the script. Instead of fighting urges, it teaches you to understand them. Developed in the 1980s by researchers at the University of Pennsylvania, CBT for weight loss targets the hidden links between your thoughts, feelings, and eating habits. A 2023 meta-analysis of 9 studies with over 900 participants found that people using CBT lost an average of 1.6 BMI points more than those on standard diets. That’s not a miracle-but it’s real, lasting change.
The 6 Cognitive Strategies That Actually Change Eating Habits
Not all CBT is the same. The most effective programs use six proven techniques, backed by clinical trials and real-world results.
- Cognitive Restructuring: This is the core. You learn to catch thoughts like "I’m a failure because I ate cake," and replace them with "One meal doesn’t define my progress." A 2017 study showed this alone reduced emotional eating by 63% in participants.
- Self-Monitoring: Writing down what you eat and how you felt before and after isn’t just busywork. People who track their meals consistently lose 5-10% more weight than those who don’t. It’s not about perfection-it’s about awareness. You can’t change what you don’t see.
- Stimulus Control: Your environment is your biggest trigger. If your kitchen is full of snacks, your brain will eat them. CBT teaches you to remove temptations: keep junk food out of the house, store meals in labeled containers, eat only at the table. Small changes, big impact.
- Goal Setting (SMART Goals): "I want to lose weight" is not a goal. A SMART goal is: "I will walk 30 minutes, 4 days a week, for the next month." Specific, measurable, achievable, relevant, time-bound. This cuts overwhelm and builds confidence one small win at a time.
- Problem-Solving for High-Risk Situations: What do you do when you’re stressed, tired, or at a party? CBT doesn’t just tell you to say no-it gives you a plan. Practice saying, "I’ll have one slice of pizza, then I’m done," or "I’ll drink water first, then decide." These scripts work because they’re pre-planned, not reactive.
- Relapse Prevention: Slip-ups aren’t failures-they’re data. CBT teaches you to analyze them: What triggered it? What thought came before? How can you respond differently next time? This turns setbacks into learning moments, not reasons to quit.
CBT vs. Other Weight Loss Methods
How does CBT stack up against the competition?
| Approach | 6-Month Weight Loss | Long-Term Retention (2 Years) | Psychological Benefits |
|---|---|---|---|
| Standard Diet & Exercise | 5.1% | 15-20% | Minimal |
| CBT Alone | 8.2% | 20-30% | 40% reduction in anxiety and depression |
| CBT + Motivational Interviewing | 12.7% | 35-40% | Significant improvement in self-worth and motivation |
| Weight-Loss Apps (Noom, WW) | 3.2% | 10-15% | Some, but limited without human support |
CBT doesn’t just help you lose weight-it helps you stop hating yourself while doing it. That’s why people who use CBT are 15% less likely to drop out of programs than those on traditional diets. The dropout rate for standard programs is 54%. For CBT, it’s 39%. The difference? CBT gives you tools, not rules.
Who Benefits Most from CBT for Weight Loss?
CBT isn’t for everyone-but it’s especially powerful for certain groups:
- People with binge eating disorder (BED): More than half of BED patients no longer meet diagnostic criteria after five years of CBT, according to a 2016 study. It doesn’t just reduce binges-it removes the shame cycle.
- Those with emotional eating: If you eat when you’re bored, stressed, or sad, CBT helps you identify the emotion and choose a different response-like calling a friend, taking a walk, or journaling.
- People who’ve tried multiple diets: If you’ve been through the cycle of losing and gaining weight, CBT breaks the pattern by fixing the root cause: your thinking.
It’s also effective for people who’ve had bariatric surgery. One study found that patients who did CBT after surgery rated their ability to stay on track improved from 2 to 7 on a 10-point scale. That’s not just weight loss-it’s life change.
What’s Holding CBT Back?
CBT works-but it’s not easy to access. There are only about 1 CBT specialist trained in obesity treatment for every 125,000 eligible patients in the U.S. Most insurance plans cover only 12 sessions, even though research shows you need 20+ for lasting results. Only 32% of U.S. plans pay for more than that.
And it takes time. It’s not a quick fix. Most people need 8 to 12 weeks just to learn how to identify distorted thoughts. Only 45% become proficient in cognitive restructuring by session six without extra support.
That’s why digital tools like Noom and WeightWatchers Beyond the Scale are growing. They use CBT principles-thought logs, cognitive reframing, goal tracking-but lack the human connection. A 2023 review found therapist-led CBT produces nearly double the weight loss of apps. The algorithm can’t replace a therapist who says, "That thought isn’t true. Let’s test it."

The Future: CBT Meets Medicine
The next big shift? Combining CBT with medications like semaglutide (Wegovy, Ozempic). These drugs reduce appetite-but they don’t fix the mental habits that led to overeating in the first place. The NIH just funded $14.7 million in research to test CBT paired with GLP-1 agonists. Early results suggest patients on both are far less likely to regain weight after stopping the drug.
This isn’t about choosing between pills and therapy. It’s about using both. Medicine handles the biology. CBT handles the brain.
How to Start CBT for Weight Loss
You don’t need to wait for a therapist to begin. Here’s how to start today:
- Track your thoughts. For three days, write down what you ate, when, and what you were thinking right before. Were you stressed? Lonely? Bored? Annoyed? Write it down.
- Spot the distortions. Look for common thinking traps: "All-or-nothing" ("I blew it, so I might as well eat everything"), "Catastrophizing" ("One cookie means I’ll gain 10 pounds"), or "Overgeneralizing" ("I always mess up").
- Challenge them. Ask: "Is this thought true? What’s the evidence for and against it? What would I say to a friend who thought this?"
- Replace it. Turn "I can never eat what I want" into "I can enjoy food without guilt if I’m mindful."
- Plan for triggers. What’s your biggest trigger? Stress? Late-night scrolling? Social pressure? Write a 3-step plan for each one.
These steps take practice. Don’t expect to master them in a week. But after a month, you’ll notice something: you’re not as controlled by your thoughts anymore. You’re starting to lead them.
Final Thought: It’s Not About Willpower
You don’t need more discipline. You need better thinking. Weight loss isn’t about starving yourself or punishing your body. It’s about learning to treat yourself with the same patience and compassion you’d give a friend. CBT doesn’t promise a perfect body. It promises a peaceful mind. And that’s the only foundation that lasts.
Is CBT for weight loss covered by insurance?
Most insurance plans cover only 12 sessions of behavioral therapy per year, and only 32% cover more than that. Some plans require a diagnosis of binge eating disorder or obesity-related health issues to approve coverage. Always check with your provider and ask if they cover CBT specifically-many only cover general counseling.
How long does CBT for weight loss take to work?
Most people start noticing changes in their eating habits after 6-8 weeks. But real, lasting results take 12-26 weekly sessions. The first few weeks focus on awareness, the middle on restructuring thoughts, and the last on building long-term habits. Rushing it reduces effectiveness.
Can I do CBT for weight loss on my own?
Yes, but with limits. Self-guided CBT books and apps can help you learn the basics-tracking thoughts, challenging distortions, setting goals. But without a trained therapist to correct your thinking patterns, you may miss key insights or reinforce unhelpful beliefs. For best results, combine self-help with occasional professional guidance.
Does CBT work for people who’ve had weight-loss surgery?
Absolutely. Many people regain weight after surgery because their old eating habits return. CBT helps them adapt to new portion sizes, manage emotional triggers, and avoid using food for comfort. Studies show patients who use CBT after surgery are significantly more likely to maintain their weight loss long-term.
What’s the biggest mistake people make with CBT for weight loss?
Thinking it’s about being perfect. CBT isn’t about never eating junk food-it’s about not letting one slip turn into a full relapse. The biggest mistake is labeling yourself a failure after a setback. CBT teaches you to see slip-ups as information, not proof you’re broken.
Do I need to be diagnosed with a mental health condition to try CBT for weight loss?
No. While CBT is often used for depression, anxiety, or binge eating disorder, you don’t need a diagnosis to benefit. Anyone struggling with emotional eating, food guilt, or inconsistent habits can use CBT techniques. It’s a tool for better thinking-not a treatment for illness.


Rod Wheatley
Wow, this is the first time I’ve seen someone actually explain why diets fail without blaming the person. I’ve been stuck in that 'I’ll start Monday' loop for years-turns out, it’s not laziness, it’s my brain screaming 'famine!' Thanks for putting this into words.