When your kidneys are damaged, high blood pressure doesn’t just worsen the problem-it speeds it up. For people with chronic kidney disease (CKD), controlling blood pressure isn’t just about avoiding heart attacks or strokes. It’s about keeping your kidneys working as long as possible. And for decades, two types of blood pressure medications have stood out as the most effective tools for this job: ACE inhibitors and ARBs.
Why Blood Pressure Matters in Kidney Disease
Your kidneys filter waste and extra fluid from your blood. When they’re healthy, they handle pressure well. But when they’re damaged-by diabetes, high blood pressure, or other causes-they become more sensitive to pressure changes. High pressure inside the kidney’s tiny filters (glomeruli) causes more damage, leaks protein into the urine, and slowly kills kidney cells.
That’s why doctors don’t just want your blood pressure to be "normal." For someone with CKD and protein in their urine, the goal is often below 130/80 mmHg. And not just any blood pressure drug will do the trick. Most lower pressure, but only ACE inhibitors and ARBs also directly protect the kidney filters.
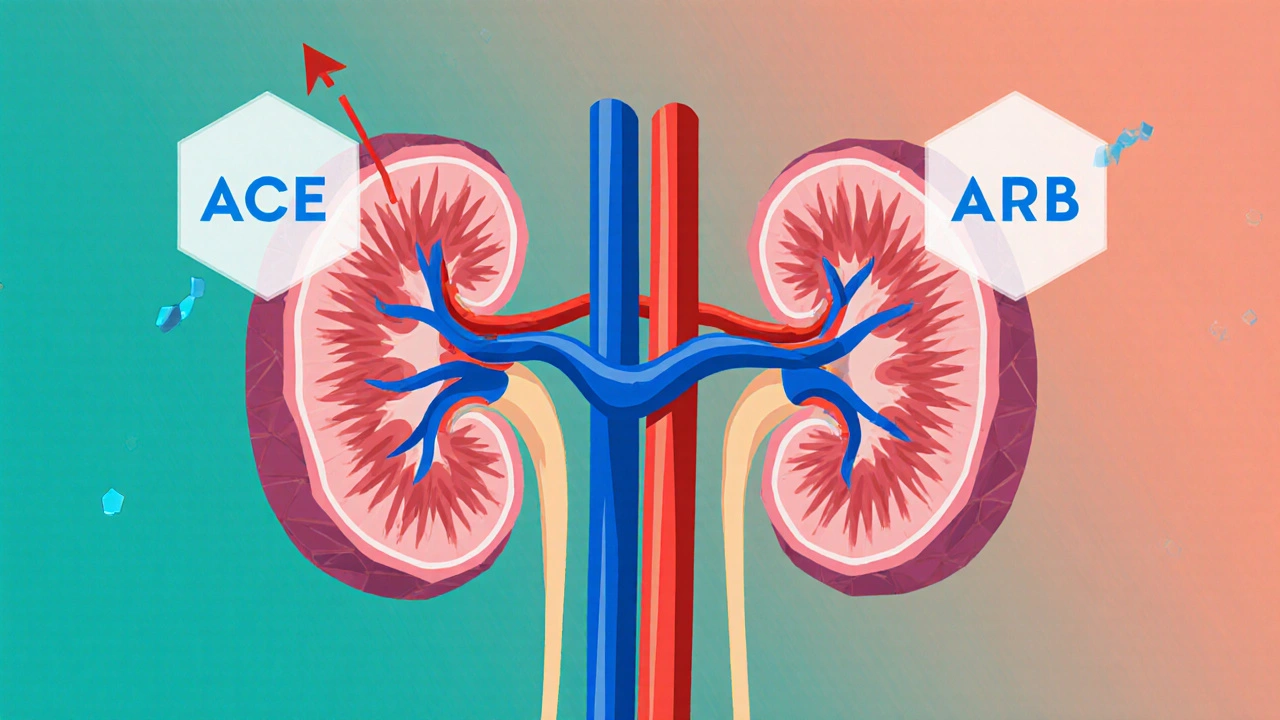
How ACE Inhibitors and ARBs Work
Both drugs target the same system: the renin-angiotensin-aldosterone system, or RAAS. This system normally helps regulate blood pressure and fluid balance. But in kidney disease, it gets overactive and starts harming the kidneys.
ACE inhibitors-like lisinopril, enalapril, and benazepril-block the enzyme that turns angiotensin I into angiotensin II. Less angiotensin II means blood vessels relax, blood pressure drops, and pressure inside the kidney filters decreases.
ARBs-like losartan, valsartan, and irbesartan-do something similar but differently. Instead of stopping angiotensin II from being made, they block its receptors. So even if angiotensin II is still around, it can’t bind to the kidney’s cells and cause damage.
The result? Both types of drugs reduce protein in the urine by 30-50%, lower blood pressure by 10-15 mmHg systolic, and slow the decline of kidney function by 20-40%. That’s not a small benefit. It can mean the difference between needing dialysis in 5 years versus 10.
ACE Inhibitors vs ARBs: What’s the Difference?
When it comes to protecting your kidneys, ACE inhibitors and ARBs are very similar in effectiveness. But they’re not the same.
ACE inhibitors are more likely to cause a dry, annoying cough-about 1 in 5 people experience it. For some, it’s mild. For others, it’s bad enough to stop taking the drug. They also carry a small risk (0.1-0.2%) of angioedema, a rare but serious swelling of the face, lips, or throat.
ARBs don’t cause cough or angioedema nearly as often. That’s why many doctors start with an ARB if a patient has had a cough with an ACE inhibitor before. But if you’ve never had side effects, ACE inhibitors are just as good-and often cheaper.
Both drugs can raise potassium levels and cause a temporary drop in kidney function when first started. That’s why doctors check your blood potassium and eGFR (a measure of kidney function) within 1-2 weeks of starting either drug. If potassium goes above 5.5 mmol/L or your eGFR drops by more than 30%, they’ll adjust the dose or pause the medication.
Can You Use These Drugs in Advanced Kidney Disease?
For years, many doctors stopped ACE inhibitors and ARBs when CKD got to stage 4 or 5 (eGFR below 30). They feared the drugs would make kidneys fail faster or cause dangerous high potassium.
But new data says otherwise.
A 2024 study of 1,237 patients with advanced CKD (average eGFR of 19.8) found those who kept taking ACE inhibitors or ARBs had a 34% lower risk of reaching kidney failure and needing dialysis. The same study found no increase in death rates-meaning the benefits outweighed the risks.
The UK-based trial that followed patients for 3 years found the same thing: those who stayed on the drugs had better kidney function over time than those who stopped. The Kidney Disease: Improving Global Outcomes (KDIGO) guidelines updated in 2023 now say: Keep using ACE inhibitors and ARBs in stage 4 and 5 CKD, as long as potassium is under 5.0 and eGFR is above 15.
The problem? Only about 58% of patients with advanced CKD are on these drugs today. Many doctors still hold back out of fear. But the evidence is clear: stopping them doesn’t protect your kidneys-it hurts them.
What About Taking Both Together?
It sounds logical-block the system at two points, get more protection. But studies show it’s not worth it.
The Veterans Affairs Nephropathy Trial found that combining an ACE inhibitor with an ARB reduced proteinuria a little more, but it also doubled the risk of acute kidney injury and increased hyperkalemia by 50%. The American Heart Association and KDIGO both strongly advise against dual therapy.
There’s no extra survival benefit. No extra kidney protection that lasts. Just more risk. Stick with one. Pick the best one for you, and use it at the highest tolerated dose.
Who Should Be on These Drugs?
You should be on an ACE inhibitor or ARB if you have:
- Chronic kidney disease (any stage) with protein in your urine (albuminuria)
- Diabetes and high blood pressure
- High blood pressure and reduced kidney function
Even if you don’t have diabetes, if your urine albumin-to-creatinine ratio (UACR) is above 200 mg/g, guidelines say you should be on one of these drugs.
But you shouldn’t start one if:
- Your potassium is already above 5.0 mmol/L
- Your eGFR is below 15 (unless you’re on dialysis)
- You’ve had angioedema from an ACE inhibitor before
- You’re pregnant

Monitoring: What You Need to Watch
These drugs are safe-but only if you’re monitored.
Here’s what your doctor should check:
- Before starting: serum potassium, eGFR, and urine protein
- 1-2 weeks after starting or increasing the dose: potassium and eGFR again
- Every 1-3 months after that: potassium and kidney function
If potassium rises above 5.5 mmol/L, your doctor may reduce the dose, prescribe a potassium binder, or adjust your diet. If your eGFR drops more than 30% from baseline, they’ll pause the drug and check for other causes-like dehydration or a blocked kidney.
Don’t skip these tests. That’s how you stay safe.
Real Patient Experiences
One patient in Melbourne, 62, with type 2 diabetes and stage 3 CKD, started lisinopril after his urine test showed heavy protein loss. His eGFR was 48. After 6 months, his protein dropped by 40%, his blood pressure stabilized at 125/75, and his kidney function stayed steady. He had no cough. He’s been on it for 4 years.
Another, 71, with stage 4 CKD, was taken off his ARB by a doctor who thought it was "too risky." His eGFR dropped from 22 to 16 in 6 months. He restarted valsartan after a second opinion. His kidney function held steady. "I thought I was doing the right thing by stopping it," he said. "Turns out, stopping was the mistake."
On Reddit’s r/kidneydisease, hundreds of people share similar stories. Many say their doctors are still hesitant. But those who’ve stuck with the drugs and monitored carefully say they feel more in control. They know their numbers. They know their limits. And they’re not rushing to dialysis.
What’s Next?
Researchers are already looking beyond ACE inhibitors and ARBs. New drugs like sacubitril/valsartan (Entresto), originally for heart failure, are showing promise in slowing kidney decline. Early data suggests it may offer even better protection than ACE inhibitors alone.
But for now, ACE inhibitors and ARBs remain the gold standard. They’re affordable, well-studied, and proven. And they’re not going away anytime soon.
If you have kidney disease and high blood pressure, ask your doctor: "Am I on the right blood pressure medicine to protect my kidneys?" If you’re not on one, ask why. If you’re off one, ask if you should get back on.
Your kidneys don’t need perfection. They just need the right protection-and these drugs have been giving it for over 40 years.
Can ACE inhibitors and ARBs reverse kidney damage?
No, they can’t reverse damage that’s already happened. But they can stop or slow further damage significantly. In many cases, patients see their proteinuria drop and their kidney function stabilize for years-sometimes decades. That’s not a cure, but it’s the closest thing to one we have.
Why do some doctors stop these drugs in advanced kidney disease?
Some doctors worry about high potassium or a sudden drop in kidney function. These risks are real, but they’re manageable with monitoring. Studies now show that stopping these drugs in advanced CKD actually leads to faster kidney decline. The fear of side effects has led to underuse-and that’s more dangerous than the side effects themselves.
Is it safe to take ACE inhibitors or ARBs with other blood pressure meds?
Yes. Most people with CKD need more than one blood pressure drug to reach their goal. ACE inhibitors or ARBs are usually the base, then doctors add diuretics, calcium channel blockers, or beta-blockers. Never combine an ACE inhibitor with an ARB-that increases risk without extra benefit.
How long does it take to see results?
Blood pressure drops within days. But kidney protection takes longer. You’ll see reduced protein in your urine after 4-8 weeks. Stable kidney function shows up over months. This isn’t a quick fix-it’s a long-term shield.
Can I stop taking these drugs if my blood pressure is normal?
No. Even if your blood pressure is under control, you should keep taking the drug if you have kidney disease and protein in your urine. The benefit isn’t just from lowering pressure-it’s from directly protecting the kidney filters. Stopping increases your risk of kidney failure.
Are there natural alternatives to ACE inhibitors and ARBs?
No. Diet, exercise, and salt reduction help manage blood pressure, but they don’t replace the kidney-protective effect of these drugs. No herb, supplement, or lifestyle change has been shown to reduce proteinuria or slow kidney decline like ACE inhibitors or ARBs. Don’t trade proven medicine for unproven remedies.

Douglas cardoza
Been on lisinopril for 3 years now. My proteinuria dropped like a rock. No cough, no issues. My doc almost didn’t want to prescribe it at first ‘cause I’m 65. Glad I pushed back.