When you take a pill for a headache or an antibiotic for an infection, you expect relief-not a life-threatening reaction. But for millions of people, common medications trigger immune responses that can turn a simple treatment into a medical emergency. Drug allergies aren’t just rare side effects; they’re real, measurable, and often misdiagnosed. The truth? Most people who think they’re allergic to penicillin aren’t. And that misunderstanding is costing lives, money, and effective treatment options.
Penicillin: The Most Misunderstood Drug Allergy
Penicillin is the most commonly reported drug allergy in the U.S., with nearly 10% of the population claiming it. But here’s the twist: over 95% of those people can actually take penicillin safely after proper testing. A study from Massachusetts General Hospital found that only 1% of people labeled with penicillin allergy truly have a confirmed IgE-mediated reaction. The rest either had a non-allergic rash, a viral infection, or outgrew the allergy years ago.Why does this matter? Because when doctors avoid penicillin due to a mislabeled allergy, they turn to broader-spectrum antibiotics like vancomycin or fluoroquinolones. These drugs are more expensive, less effective against common infections, and contribute to antibiotic resistance. A 2017 JAMA study showed patients with a penicillin allergy label stayed in the hospital half a day longer and paid over $1,000 more per admission. That adds up to $1.2 billion a year in unnecessary costs across the U.S.
Testing for penicillin allergy is straightforward and highly accurate. Skin testing combined with a small oral dose of amoxicillin is 97-99% reliable. The test takes a few hours and is done in an allergist’s office. If you were told you’re allergic as a child and haven’t taken penicillin since, there’s a very good chance you’re no longer allergic. The immune system forgets. Many people outgrow their penicillin allergy after 10 years without exposure.
Other Antibiotics That Trigger Reactions
Penicillin isn’t alone. Other antibiotics, especially beta-lactams like cephalosporins and carbapenems, can also cause allergic reactions. But cross-reactivity isn’t as common as once thought. While older studies claimed up to 10% of penicillin-allergic people react to cephalosporins, modern data shows it’s closer to 1-3%. That means most people can safely take these drugs-even if they’ve had a penicillin reaction.Sulfa drugs are another major trigger. Trimethoprim-sulfamethoxazole (Bactrim) is one of the most prescribed antibiotics for urinary tract infections, but it causes reactions in about 3% of the general population. For people with HIV, that number jumps to 60%. Reactions range from mild rashes to life-threatening conditions like Stevens-Johnson Syndrome. Unlike penicillin allergies, sulfa reactions don’t always involve IgE. They’re often T-cell mediated, meaning they can show up days later, making them harder to link to the drug.
Quinolones like ciprofloxacin and levofloxacin are also frequently blamed for allergic reactions. But many of these are actually non-allergic side effects-nausea, dizziness, or tendon pain. True IgE-mediated reactions to quinolones are rare. Still, patients often avoid them out of fear, limiting treatment options for stubborn infections.
NSAIDs: More Than Just Stomach Upset
Ibuprofen, naproxen, and aspirin are in nearly every medicine cabinet. But for some, they’re dangerous. Nonsteroidal anti-inflammatory drugs (NSAIDs) cause allergic-like reactions in about 1 in 100 people. That might sound low, but it adds up to hundreds of thousands of reactions each year in the U.S. alone.Aspirin is a special case. In 7% of adults with asthma and 14% of those with nasal polyps, aspirin triggers a unique condition called aspirin-exacerbated respiratory disease (AERD). This isn’t a classic allergy. It’s a metabolic imbalance where the body overproduces inflammatory chemicals after taking aspirin or other NSAIDs. Symptoms include severe wheezing, nasal congestion, and sometimes anaphylaxis. People with AERD must avoid all NSAIDs-not just aspirin.
Unlike penicillin, there’s no skin test for NSAID allergies. Diagnosis relies on history and sometimes an oral challenge under medical supervision. If you’ve ever had trouble breathing after taking Advil or Aleve, don’t assume it’s just indigestion. Talk to an allergist. There are safe alternatives like acetaminophen or COX-2 inhibitors that won’t trigger the same reaction.

Anticonvulsants and Genetic Risk
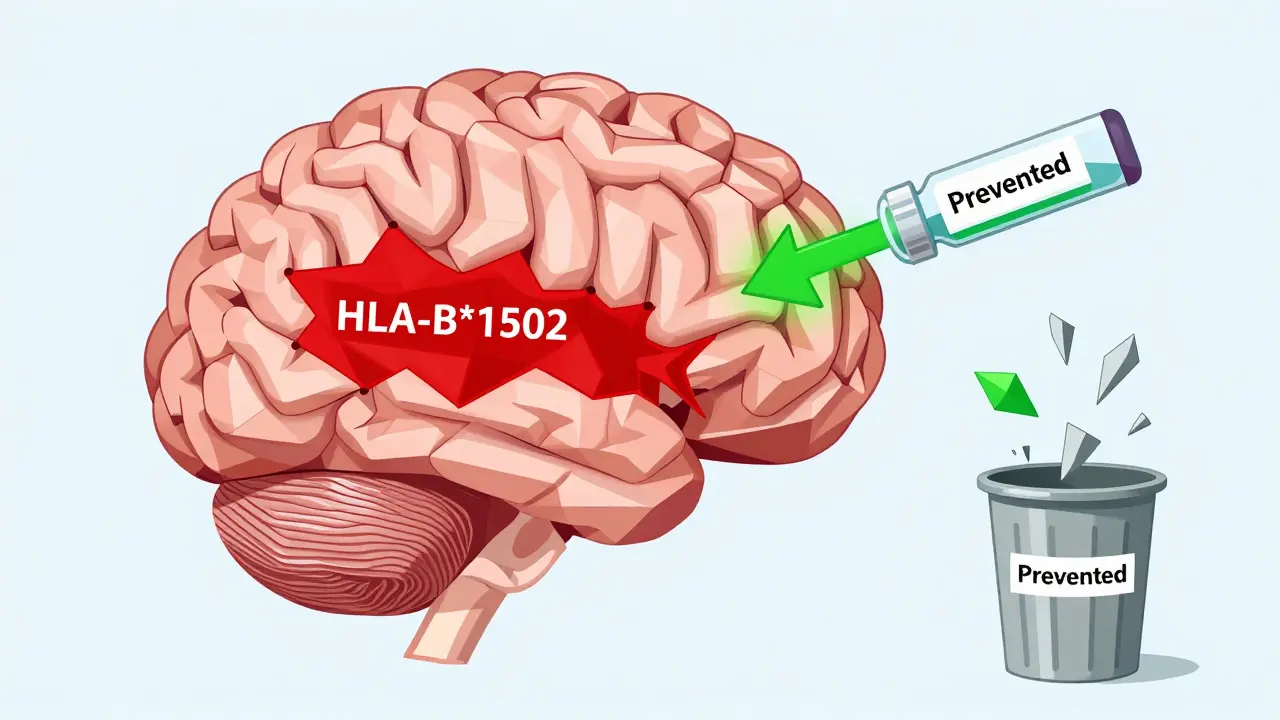
Carbamazepine (Tegretol), used for epilepsy and nerve pain, is one of the most dangerous drugs for certain populations. In Southeast Asian communities-especially people of Han Chinese, Thai, or Malaysian descent-carbamazepine can trigger Stevens-Johnson Syndrome (SJS) or toxic epidermal necrolysis (TEN). These are devastating skin reactions that cause blistering, peeling, and can be fatal.The reason? A genetic marker called HLA-B*1502. People with this gene variant have a 100-fold higher risk of developing SJS/TEN when taking carbamazepine. That’s why the FDA recommends genetic testing before prescribing it in high-risk groups. In Taiwan, where screening became routine, SJS/TEN cases dropped by 90%. This isn’t theoretical-it’s life-saving.
Lamotrigine (Lamictal) is another anticonvulsant linked to rashes. About 5-10% of users develop a rash, and in 0.8 out of every 1,000 patients, it turns serious. The risk is highest in the first few weeks of use. Doctors now start with low doses and increase slowly. If you get a rash while starting lamotrigine, don’t ignore it. Stop the drug and call your doctor immediately.
Chemotherapy and Biologics: The New Frontier
Cancer treatments are among the most likely to cause hypersensitivity. Taxanes like paclitaxel (Taxol) trigger reactions in 20-41% of patients. Monoclonal antibodies like cetuximab (Erbitux) cause infusion reactions in up to 23% of users, with 2% experiencing severe anaphylaxis.These aren’t classic allergies. They’re often caused by immune activation during infusion-not IgE. But the symptoms-rash, low blood pressure, trouble breathing-look identical. Hospitals now premedicate patients with steroids and antihistamines before giving these drugs. In many cases, they can still be given safely, even after a prior reaction, using a slow, graded infusion protocol.
Biologics are on the rise. As more of these targeted therapies enter the market, we’ll see more hypersensitivity cases. Experts predict we’ll need 20% more allergists by 2030 just to manage these reactions. It’s not just about the drugs-it’s about the system behind them.
Contrast Dyes and Diagnostic Risks
If you’ve had a CT scan or MRI with contrast dye, you might have heard you’re allergic. But true allergies to iodinated contrast media are rare-only 1-3% of patients have any reaction, and severe ones are less than 0.04%. Most reactions are just mild flushing or nausea, not true allergies.Still, because the symptoms can mimic anaphylaxis, doctors often label these patients as “allergic.” That leads to unnecessary avoidance of future scans or use of less effective imaging methods. The good news? Premedication with steroids and antihistamines reduces moderate-to-severe reactions from 12.7% to just 1%. If you’ve had a reaction before, you can still safely get contrast dye-with the right prep.
Why Mislabeling Is a Public Health Crisis
The biggest problem isn’t the allergies themselves-it’s how we handle them. A 2022 survey found that 68% of people with drug allergy labels never got tested. Most don’t know testing exists. Others assume it’s too expensive, too risky, or too complicated.But here’s what’s clear: every mislabeled allergy leads to worse outcomes. Patients get broader-spectrum antibiotics, which fuel superbugs. They miss out on first-line treatments that work better and cost less. And they live with unnecessary fear.
Health systems are starting to fix this. Telehealth penicillin allergy clinics now cut wait times from 60 days to under two weeks. Electronic health records are being updated to flag low-risk labels. Pharmacists are trained to ask: “When was your last reaction? Did you ever get tested?”
The message is simple: if you think you’re allergic to a medication, don’t assume. Ask. Get tested. Your next prescription-and maybe your life-depends on it.
What You Should Do Now
- If you’ve been told you’re allergic to penicillin, ask your doctor about allergy testing. It’s safe, quick, and often covered by insurance.
- If you had a rash after taking an antibiotic as a child, you may no longer be allergic. Reactions fade over time.
- Don’t avoid NSAIDs just because you think you’re allergic. See an allergist if you’ve had breathing issues after taking aspirin or ibuprofen.
- If you’re prescribed carbamazepine and have Southeast Asian ancestry, ask about HLA-B*1502 genetic testing before starting.
- Keep a written list of all drug reactions you’ve had-including symptoms, timing, and what you were taking. This helps doctors make better decisions.
Can you outgrow a drug allergy?
Yes, many people outgrow drug allergies, especially penicillin. Studies show that 80% of people labeled with penicillin allergy as children lose their sensitivity after 10 years without exposure. The immune system can forget the reaction. Testing with skin tests and oral challenges confirms whether the allergy is still active.
Is a rash always a sign of a drug allergy?
No. Many rashes that appear after taking a drug are not allergic. Viral infections, heat, or even side effects can cause rashes that look like allergies. True drug allergies usually involve other symptoms like swelling, trouble breathing, low blood pressure, or blistering skin. Delayed rashes (appearing 3-10 days later) are often T-cell mediated, not IgE, and still need medical evaluation.
Are all antibiotic allergies the same?
No. Penicillin allergies are often IgE-mediated and can cause anaphylaxis. Sulfa drug reactions are usually T-cell mediated and appear days later. Quinolone reactions are often non-allergic side effects. Each requires a different approach to diagnosis and management. Don’t assume one allergy means you’re allergic to all antibiotics.
Can I take cephalosporins if I’m allergic to penicillin?
Yes, in most cases. Cross-reactivity between penicillins and cephalosporins is now estimated at only 1-3%, not the outdated 10%. If your penicillin reaction was mild (like a rash), you can likely take cephalosporins safely. If it was severe (anaphylaxis), consult an allergist before trying one. Skin testing or a supervised challenge may be recommended.
What’s the difference between an allergy and a side effect?
An allergy involves your immune system reacting to the drug as if it’s a threat. Symptoms include hives, swelling, wheezing, or anaphylaxis. Side effects are predictable, non-immune reactions-like nausea from antibiotics or dizziness from blood pressure meds. Side effects are common and not dangerous for most people. Allergies are rare and can be life-threatening.

Patrick Jarillon
So let me get this straight - we’re being told to trust doctors who labeled me allergic to penicillin when I was 5 and haven’t touched it since… but now they want me to swallow a pill in their office like it’s a dare? 🤨
Meanwhile, the pharmaceutical companies are quietly laughing because they’ve been pushing vancomycin for 20 years - it’s like 3x the price and they get to sell more.
And don’t even get me started on the HLA-B*1502 test - why’s it only mandatory in Taiwan but not here? Coincidence? Or is Big Pharma just happy we’re all too busy scrolling TikTok to ask questions?
I’ve got a cousin in Bangalore who got SJS from carbamazepine - his skin peeled off like a banana. They didn’t test him. He’s lucky to be alive. Now they say ‘genetic testing is expensive.’ Nah. It’s profitable to keep you scared and prescribing the expensive stuff.
And yes, I’ve been told I’m ‘overreacting.’ I’ve been told that since I was 12. I’m not overreacting. I’m just the only one who read the damn study.