Imagine waking up with your eye burning like it’s full of sand, light hurting your vision, and a white spot you can’t ignore. This isn’t just a bad day-it could be a corneal ulcer, a serious open sore on the clear front surface of your eye. For contact lens wearers, this isn’t rare. Around 1 in 500 people who wear contacts get one each year. If you sleep in them? That risk jumps to 1 in 50. And if you don’t act fast, you could lose vision permanently.
What Exactly Is a Corneal Ulcer?
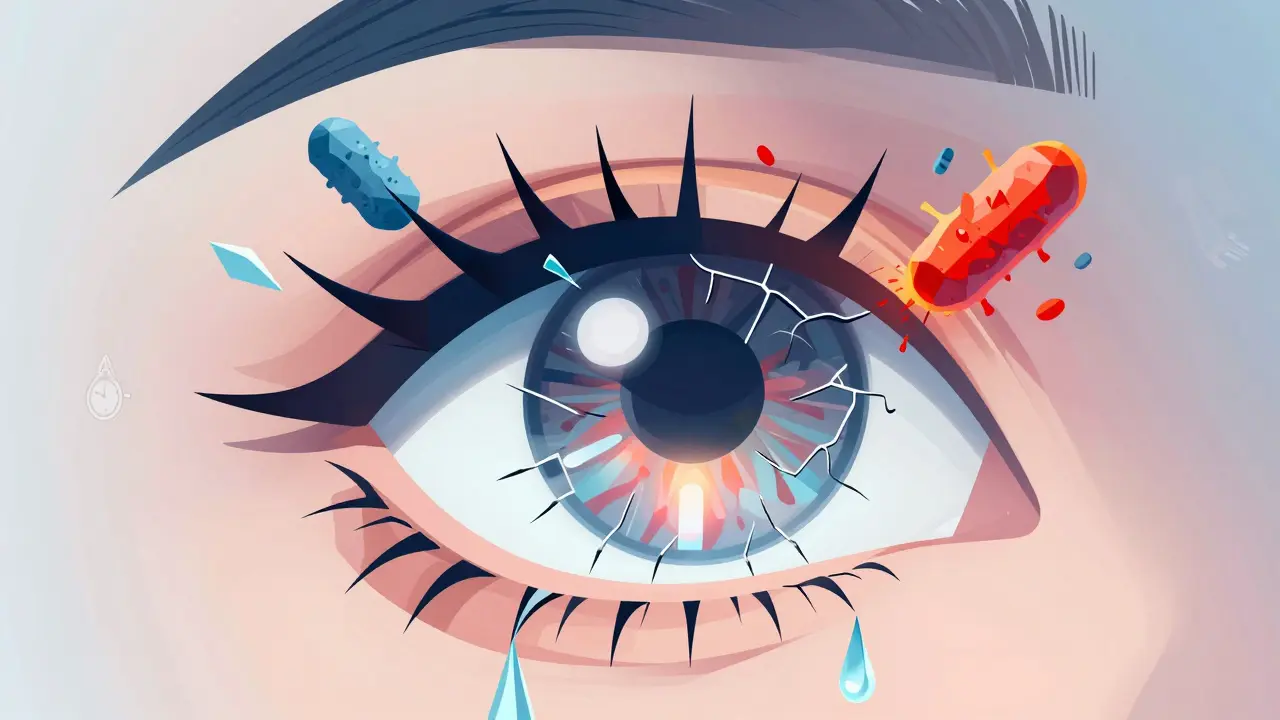
The cornea is the clear, dome-shaped surface covering your iris and pupil. It’s tough, but it’s not invincible. A corneal ulcer is an open wound on this layer, usually caused by an infection that eats away at the tissue. It’s not the same as a scratch (called a corneal abrasion), which is just a surface scrape that heals on its own. An ulcer is deeper. It’s like a crater forming on your eye’s front window-and it’s often infected with bacteria, fungi, or even a tiny parasite called Acanthamoeba. Contact lenses are the biggest trigger. They sit right on the cornea, blocking oxygen and trapping germs. Every time you touch your lenses with dirty fingers, rinse them with tap water, or sleep in them, you’re increasing the chance of something nasty getting stuck underneath. The FDA calls corneal ulcers one of the most dangerous risks of contact lens use. And they’re not exaggerating. Left untreated, these ulcers can scar the cornea, cause clouded vision, or even lead to blindness.Why Contact Lenses Increase Your Risk So Much
You might think modern lenses are safer, and they are-but they’re not risk-free. Soft contact lenses, especially the kind designed for overnight wear, are the biggest problem. Here’s why:- They block oxygen. Your cornea doesn’t have blood vessels-it gets oxygen from the air. A lens sitting on it all night cuts off that supply, making it easier for infections to take hold.
- They trap germs. Bacteria from your fingers, your pillow, or even your tap water can stick to the lens and get pushed against your eye.
- They create a perfect breeding ground. Moisture, warmth, and trapped debris? That’s a party for microbes.
- Scratched or damaged lenses
- Using tap water or homemade solutions to clean lenses
- Wearing lenses while swimming, showering, or in hot tubs
- Having dry eyes, blepharitis (eyelid inflammation), or conditions like Bell’s palsy that stop your eyelids from closing fully
- Using steroid eye drops without medical supervision-they can hide infection while letting it spread
What It Feels Like: The Warning Signs You Can’t Ignore
The problem with corneal ulcers is they don’t always start with obvious symptoms. At first, you might think it’s just tired eyes or a bit of irritation. But here’s what it really looks and feels like:- Severe eye pain-often described as a constant, deep ache
- Red, bloodshot eyes that don’t improve with drops
- Blurry, hazy, or cloudy vision
- White or gray spot on the cornea (you might see it in the mirror)
- Excessive tearing or thick, yellow/green discharge
- Extreme sensitivity to light-bright lights feel like a knife to the eye
- Feeling like something’s stuck in your eye-even when there’s nothing there

How Doctors Diagnose a Corneal Ulcer
If you go to an eye doctor with these symptoms, they won’t just look at your eye. They’ll run tests. Here’s what happens:- Fluorescein staining: A yellow dye is dropped into your eye. Under blue light, any damage on the cornea glows green. It’s quick, painless, and shows exactly where the ulcer is.
- Slit-lamp exam: A high-powered microscope with a bright light lets the doctor zoom in on the ulcer’s size, depth, and shape.
- Corneal scraping: If the ulcer looks serious, they’ll gently scrape a tiny bit of tissue from the edge. That sample goes to a lab to find out if it’s bacterial, fungal, or viral.
- Visual acuity test: They’ll check how well you can see with and without your lenses.
- Keratometry: Measures the curve of your cornea to see if it’s warped from the damage.
How It’s Treated: Speed Is Everything
Time is vision. The sooner you start treatment, the less likely you are to end up with permanent scarring. Treatment depends on what’s causing the ulcer:- Bacterial ulcers: The most common type. Treated with antibiotic eye drops-usually fluoroquinolones like ciprofloxacin or moxifloxacin. You might need to use them every hour at first.
- Viral ulcers: Often caused by herpes simplex virus. Treated with antiviral drops like acyclovir.
- Fungal ulcers: Rare but dangerous. Often from contaminated solutions or water exposure. Treated with antifungal drops like natamycin or voriconazole.
- Acanthamoeba: A tough parasite from tap water or pools. Requires long-term, aggressive treatment with special drops and sometimes oral meds.
How to Prevent a Corneal Ulcer
The best treatment is no treatment. Prevention works. Here’s how:- Never sleep in your lenses. Even if they’re labeled “extended wear,” skip the overnight wear. It’s the #1 preventable risk.
- Wash your hands before touching your lenses. Soap and water. Dry with a lint-free towel.
- Use only approved cleaning solutions. Never use water-tap, bottled, or distilled. Never reuse solution. Always fresh.
- Replace lenses on schedule. Daily disposables? Toss them every day. Monthly? Don’t stretch them to six weeks.
- Take your lenses out before swimming or showering. If you can’t, wear tight-fitting goggles.
- Give your eyes a break. Wear glasses at least one day a week. Let your cornea breathe.
- Don’t use steroid drops unless prescribed. They can mask infection and make it worse.
When to Go to the Emergency Eye Clinic
You don’t need to wait for your regular appointment. If you have:- Sudden vision loss
- Intense pain that doesn’t improve
- A visible white spot on your eye
- Light sensitivity so bad you can’t open your eye
Final Thought: Your Eyes Can’t Wait
Contact lenses are convenient. They’re safe-when used right. But they’re not toys. They’re medical devices. And like any medical device, misuse has consequences. Corneal ulcers don’t come with warning labels you can ignore. They come with pain, fear, and the real chance of blindness. If you wear contacts, know the signs. Know the risks. And if something feels off? Act like your vision depends on it-because it does.Can a corneal ulcer heal on its own?
No. A corneal ulcer is an infected open sore that won’t heal without medical treatment. Even if the pain seems to go away, the infection can keep spreading under the surface. Delaying treatment increases the risk of permanent scarring or vision loss.
Are daily disposable contacts safer than monthly ones?
Yes, generally. Daily disposables reduce the chance of bacteria buildup because you throw them out every day. Monthly lenses require cleaning and storage, which introduces more opportunities for contamination-even with careful use. If you’ve had an infection before, daily lenses are the safer choice.
Can I still wear contacts after having a corneal ulcer?
Maybe-but only after your eye doctor says it’s safe. You’ll need to wait until the ulcer is fully healed, which can take weeks or months. Your doctor may recommend switching to daily disposables or limiting wear time. Never resume wearing lenses without a professional go-ahead.
Is it safe to swim with contact lenses?
No. Water-whether from pools, lakes, showers, or hot tubs-can carry dangerous microbes like Acanthamoeba. Even if you rinse your lenses afterward, the damage is already done. Always remove lenses before swimming or wear waterproof goggles.
Do steroid eye drops help corneal ulcers?
Only under strict medical supervision. Steroids reduce inflammation, but they also suppress the immune system. If used too early or without knowing the cause of the infection, they can make bacterial or fungal ulcers worse. Never use steroid drops without a doctor’s prescription.
How long does it take to recover from a corneal ulcer?
Mild ulcers can heal in 1-2 weeks with proper treatment. Severe cases, especially fungal or Acanthamoeba infections, can take months. Scarring may remain, affecting vision. Recovery time depends on the cause, size, how fast treatment started, and your overall eye health.

Hilary Miller
I wore contacts for 10 years and never thought twice until I woke up with my eye on fire. Don't sleep in them. Just don't. I'm lucky I didn't lose vision.