When your stomach won’t empty properly, eating becomes a chore-not a pleasure. You finish a small meal and feel like you’ve eaten a feast. Nausea hits. Bloating sticks. Vomiting comes without warning. This isn’t just indigestion. This is gastroparesis: a condition where the stomach muscles don’t work right, and food lingers for hours, sometimes days, instead of moving into the small intestine. It’s not rare. About 4% of people have it, and it’s far more common in women and those with long-term diabetes. The good news? You can take control-with the right diet, habits, and support.
What Gastroparesis Really Feels Like
Most people think nausea and bloating are normal after a big meal. But with gastroparesis, these symptoms don’t go away. They’re constant. You feel full after just a few bites. Even water can feel too much. You might vomit undigested food hours after eating. Abdominal pain is common, and so is heartburn-because food and acid sit too long and back up into the esophagus. Symptoms don’t come and go randomly. They follow a pattern. Studies show 90% of people with gastroparesis have nausea. About 85% feel full too quickly. Vomiting happens in 75-80%. And if you’ve had these symptoms for three months or longer, it’s not just a bad stomach bug-it’s likely gastroparesis. The worst part? It’s invisible. No one can see how much you’re struggling. You cancel plans because you’re scared of getting sick. You skip family dinners. You lose weight without trying. And if you have diabetes, your blood sugar swings wildly because food isn’t moving on schedule. It’s not just about food. It’s about your whole life.Why Your Stomach Stops Working
Your stomach doesn’t just hold food-it churns it. That’s done by nerves and muscles working together. The vagus nerve, which runs from your brain to your stomach, tells the muscles when to contract. When that nerve gets damaged, the stomach doesn’t get the signal. In 70% of cases, that nerve damage comes from diabetes. High blood sugar over years slowly harms the nerves. In 35% of cases, gastroparesis is caused by diabetes. Another 30% have no known cause-called idiopathic gastroparesis. Some cases follow surgery, especially stomach or esophageal procedures. Others are tied to autoimmune conditions like scleroderma. It’s not just nerves. Sometimes the stomach muscles themselves are weakened. That’s less common-about 15% of cases-but it still means the stomach can’t squeeze food forward. The result? Food stays. Ferments. Turns into hard lumps called bezoars. Or it backs up, causing infection, dehydration, or malnutrition.How Doctors Diagnose It
There’s no single blood test for gastroparesis. Diagnosis means ruling out blockages-like tumors or strictures-and proving food moves too slowly. The gold standard is a gastric emptying scan. You eat a meal with a tiny bit of radioactive material. Then, doctors take pictures over 4 hours to see how fast it leaves your stomach. The rule? If less than 40% of the meal is gone after two hours, you have gastroparesis. Some centers use stricter criteria, especially for adults. Children’s hospitals use different benchmarks, but the principle is the same: delayed emptying. Other tests help too. An upper endoscopy checks for physical blockages. An ultrasound or CT scan can spot bezoars. And some clinics now use breath tests or wireless motility capsules that track how food moves through your whole gut. But here’s the catch: symptoms don’t always match test results. Some people have severe symptoms but normal emptying. Others have slow emptying but feel fine. That’s why doctors look at the whole picture-your history, your diet, your symptoms, and your response to treatment.The Diet That Actually Works
Diet isn’t just advice-it’s the first line of defense. Studies show 65% of people get better just by changing what and how they eat. No drugs. No surgery. Just smarter meals. Start small. Eat 5 to 6 tiny meals a day instead of 3 big ones. Each meal should be 1 to 1.5 cups max. That’s about the size of a coffee mug. Bigger portions overwhelm your stomach. Avoid fat. High-fat foods slow emptying by 30-50%. That means fried food, butter, cream, cheese, fatty meats, and even avocado. Stick to lean proteins like skinless chicken, fish, tofu, and egg whites. Cut fiber. Raw veggies, whole grains, nuts, seeds, and fruit skins are hard to break down. They turn into stubborn lumps. Cook everything. Blend it. Strain it. Mashed potatoes, applesauce, strained soups, and well-cooked carrots are fine. Avoid broccoli, cauliflower, corn, peas, and raw apples. Skip carbonation. Soda, sparkling water, and beer inflate your stomach. That extra gas makes bloating worse. Stick to still water, weak tea, or broth. Separate solids and liquids. Drink fluids 30 minutes before or after meals-not with them. Mixing them increases stomach volume by 40%, which triggers nausea. Sip water slowly-1 to 2 ounces every 15 minutes throughout the day. Big gulps = more discomfort. Blend it. If chewing doesn’t help, blend your food until it’s smooth. A particle size under 2mm is ideal. That means blending cooked chicken with broth, or applesauce with yogurt. Many people see 70% symptom relief just by switching to blenderized meals.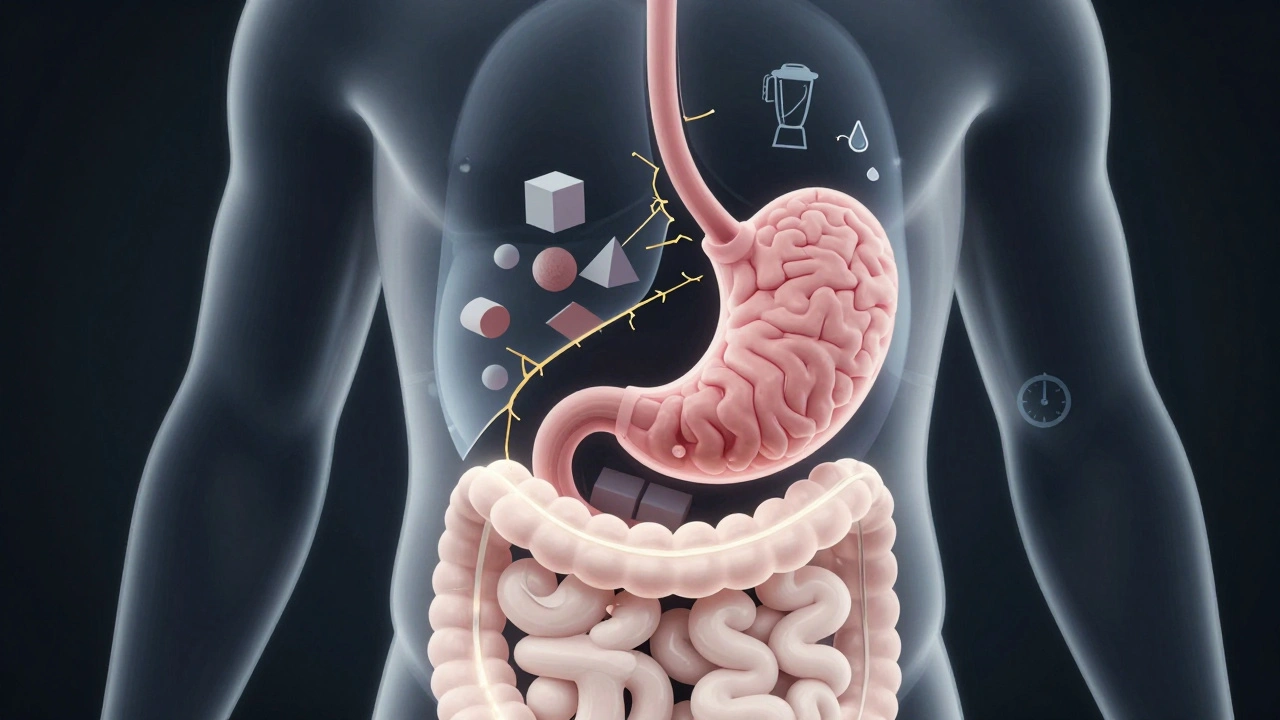
What to Eat: A Simple Daily Plan
You don’t need fancy recipes. You need simple, digestible foods.- Breakfast: Scrambled eggs with cooked spinach, blended into a smoothie with a banana and almond milk (unsweetened)
- Mid-morning snack: Applesauce or canned peaches in juice (no syrup)
- Lunch: Chicken noodle soup (strained, no chunks), white rice, steamed carrots
- Afternoon snack: Greek yogurt (low-fat, no fruit pieces), a spoon of honey
- Dinner: Baked salmon, mashed sweet potato, pureed peas
- Evening snack (if needed): A small cup of broth or a gelatin dessert
When Diet Isn’t Enough
If you’ve tried everything and still feel sick, it’s time for the next step. Medications can help. Metoclopramide is the most common. It helps the stomach contract and move food along. But it has a serious risk: tardive dyskinesia. That’s uncontrolled face or body movements that can be permanent. Doctors limit it to short-term use-usually under 12 weeks. Domperidone is another option. It’s not FDA-approved in the U.S. but available through special programs. It works without the same brain side effects. Talk to your doctor about it. For severe cases, there’s gastric electrical stimulation (GES). It’s like a pacemaker for your stomach. A small device is implanted under the skin. It sends mild pulses to the stomach muscles. In 70% of people, vomiting drops by more than half. It’s not a cure, but it gives back control. A newer option is per-oral pyloromyotomy (POP). A scope is inserted through the mouth. The muscle at the bottom of the stomach (the pylorus) is cut to let food pass more easily. Success rates are 60-70%. It’s minimally invasive and doesn’t require open surgery.Complications You Can’t Ignore
Left untreated, gastroparesis doesn’t just make you uncomfortable-it’s dangerous. Bezoars form in 6% of cases. These are hard masses of undigested food. They can block the stomach. Some need endoscopy to remove. A few require surgery. Dehydration happens in 25% of moderate to severe cases. Constant vomiting drains your fluids. Electrolytes like potassium drop. That can cause heart rhythm problems. Malnutrition hits 30-40% of long-term patients. You’re not eating enough because you’re sick. You lose weight-10% or more of your body weight. Your muscles weaken. Your immune system suffers. And if you have diabetes? Your blood sugar goes wild. Food sits. Then suddenly moves. Glucose spikes. You get highs and lows without warning. It’s hard to manage insulin. Many patients end up in the hospital. Hospital stays average 5.2 days per admission. And with 3.5 hospitalizations per patient each year, the burden is real.


Maria Elisha
I tried the blenderized meals thing and it was a game changer. No more vomiting after dinner. Just blend everything, even the chicken. Life’s weird but this works.