Imagine your body storing 10 times more iron than it should. Not from eating too much steak. Not from taking supplements. But because your genes won’t let you stop absorbing it. That’s hemochromatosis-a silent, genetic condition that slowly poisons your liver, heart, and pancreas with iron. It’s not rare. In Australia, about 1 in 200 people of Northern European descent carry the gene mutation that causes it. And most don’t know they have it until it’s too late.
What Exactly Is Hemochromatosis?
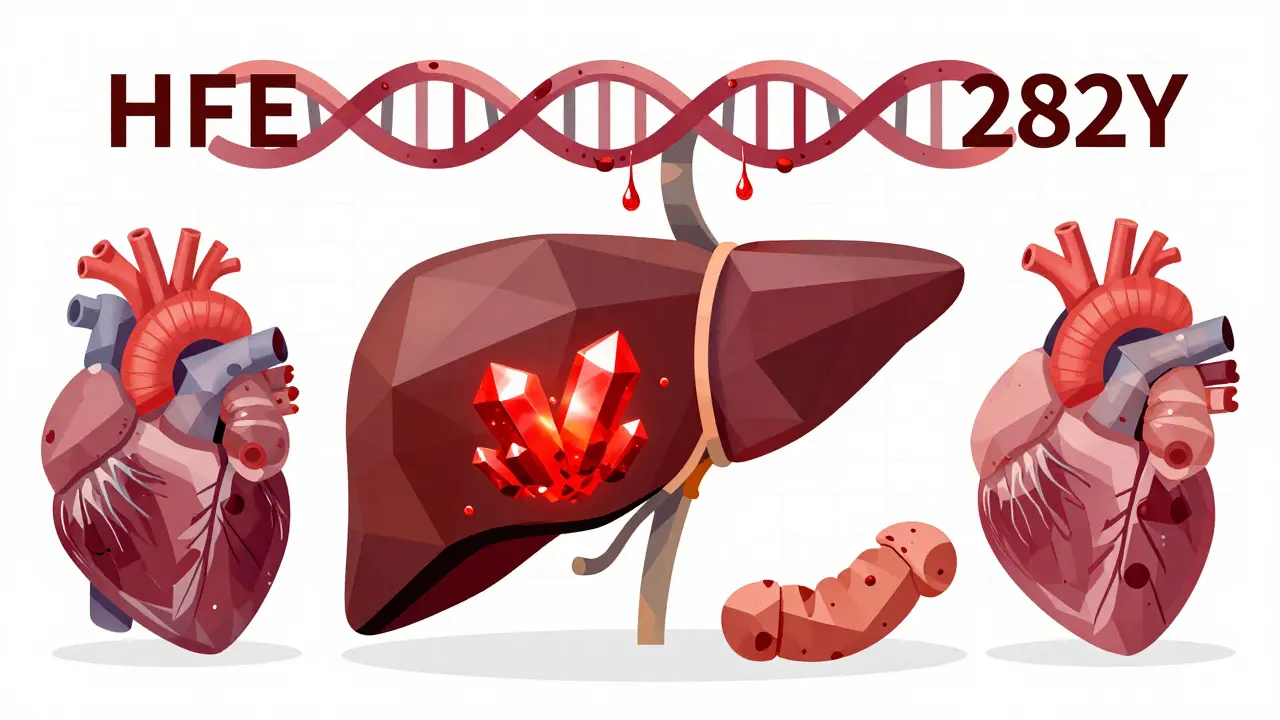
Hemochromatosis isn’t just "too much iron." It’s a genetic flaw that turns your body into an iron sponge. Normally, your gut absorbs just enough iron from food to replace what you lose through blood loss, sweat, and skin cells. But if you have two copies of the mutated HFE gene-especially the C282Y variant-your body keeps absorbing iron even when it’s full. That iron doesn’t get flushed out. It piles up in your liver, heart, pancreas, and joints.
This isn’t a new discovery. Doctors noticed patients with dark skin and liver problems as far back as 1865. But it wasn’t until 1996 that scientists found the root cause: a broken gene that stops the liver from making enough hepcidin. Hepcidin is the hormone that tells your gut, "Stop taking in iron." When it’s missing, your body keeps absorbing-and storing-iron like there’s no tomorrow.
How Do You Know You Have It?
The problem? Early symptoms are easy to ignore. Fatigue? Everyone gets tired. Joint pain? Maybe you’re just getting older. Loss of libido? Stress. But if you’re a man over 30 and you’re constantly exhausted, your knuckles ache, and you feel like you’ve lost your spark, it’s worth checking.
Here’s what doctors look for:
- Serum ferritin above 300 ng/mL in men, or 200 ng/mL in women
- Transferrin saturation over 45%
- Genetic test confirming HFE mutations (C282Y homozygous is the most common)
Most people don’t get tested until they’re in trouble. By then, they’ve got bronze-tinted skin, diabetes, or liver scarring. One study found that 68% of patients saw 3 to 5 doctors over 5 to 7 years before getting the right diagnosis. That’s not because doctors are careless-it’s because the symptoms look like everything else.
Why the Liver Takes the First Hit
Your liver is the main storage site for iron. When iron builds up, it doesn’t just sit there. It triggers inflammation, oxidative stress, and cell death. Over time, that leads to fibrosis-scar tissue replacing healthy liver cells. Once cirrhosis sets in, your liver can’t regenerate. And cirrhosis raises your risk of liver cancer by 20 times.
Here’s the scary part: if your ferritin level is above 1,000 ng/mL when you’re diagnosed, you have a 50-75% chance of already having cirrhosis. And once cirrhosis is there, phlebotomy won’t reverse it. It can stop further damage-but it can’t undo what’s already done.
That’s why early detection is everything. A person diagnosed before ferritin hits 1,000 has a 95% chance of living a normal lifespan. Someone diagnosed after cirrhosis develops? Survival drops to 60% over 10 years.
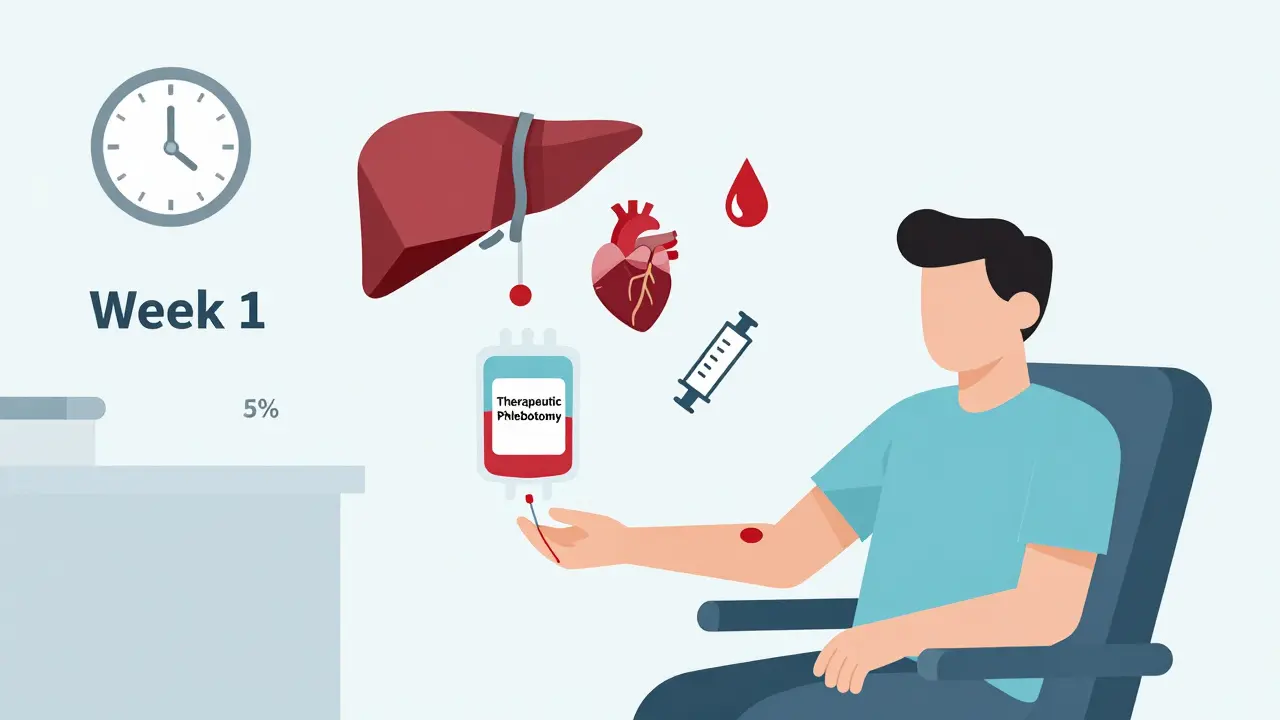
Phlebotomy: The Simple, Free Treatment That Works
Here’s the good news: hemochromatosis is one of the few genetic diseases you can treat with a needle and a blood bag.
Therapeutic phlebotomy is exactly like donating blood-but it’s medically required, not voluntary. Each session removes about 450-500 mL of blood, which contains roughly 200-250 mg of iron. Your body doesn’t replace that iron right away. It has to pull it from your stores. Slowly, over weeks and months, your iron levels drop.
The process has two phases:
- Induction phase: Weekly blood removal until ferritin hits 50 ng/mL. For someone with ferritin at 3,000, that might take 60+ sessions over 18 months.
- Maintenance phase: Every 2 to 4 months, you get a blood draw to keep ferritin between 50 and 100 ng/mL. Most people need 4 to 6 sessions a year.
It’s cheap. It’s effective. And it’s covered by most insurance. Each session costs $0 to $50. Compare that to iron-chelating drugs like deferasirox, which cost $25,000 to $35,000 a year and come with nasty side effects-nausea, kidney damage, heart rhythm issues.
One Reddit user, u/HemoWarrior, shared: "After 8 years of pain, my ferritin was 2,850. I needed 62 sessions. But now? I sleep through the night. My joints don’t ache. I feel like I’m 30 again."
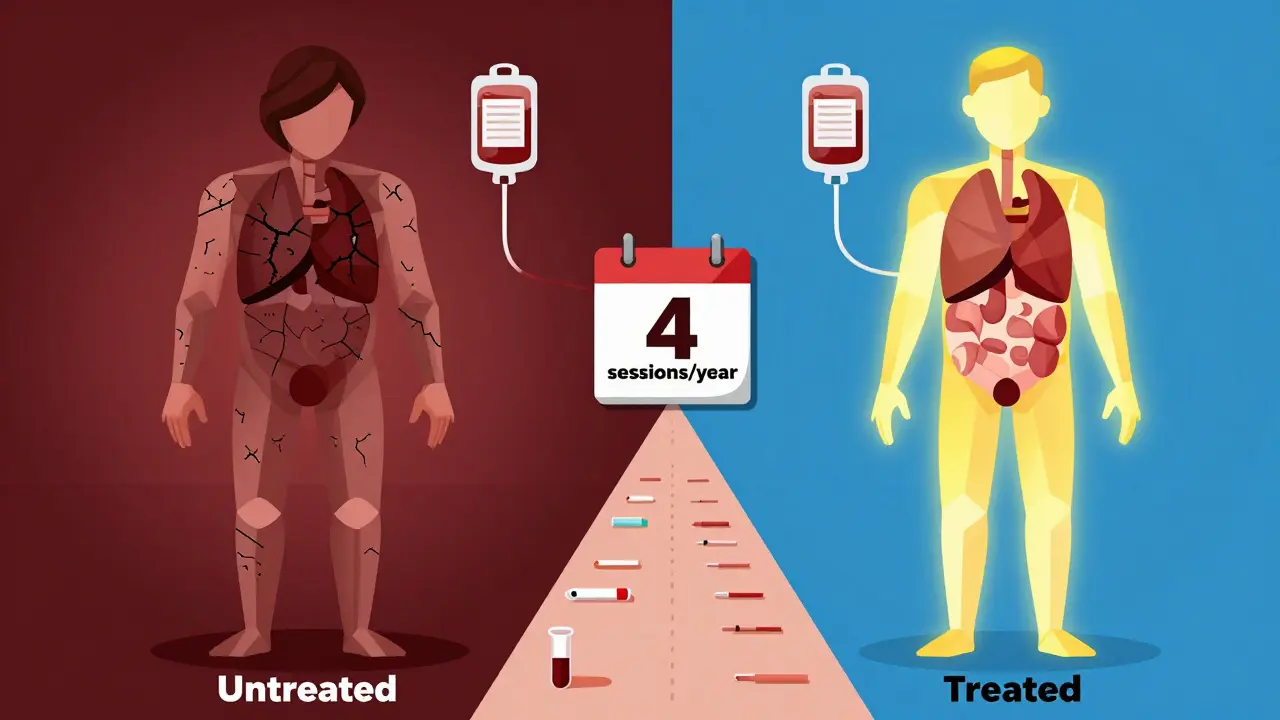
What Happens If You Don’t Treat It?
Untreated hemochromatosis doesn’t just hurt your liver. It attacks multiple organs:
- Liver: Fibrosis → cirrhosis → liver cancer
- Pancreas: Iron damages insulin-producing cells → type 2 diabetes (affects 25% of untreated patients)
- Heart: Iron buildup can cause arrhythmias or heart failure
- Testicles and Pituitary: Low testosterone, loss of libido, erectile dysfunction (affects 54% of men)
- Joints: Iron crystals form in cartilage → arthritis, especially in knuckles
And here’s the kicker: women are protected for years because they lose iron through menstruation. But after menopause, their risk spikes. That’s why many women aren’t diagnosed until their 60s-when it’s already too late.
Who Should Get Tested?
You don’t need to be sick to get tested. If any of these apply to you, ask your doctor for a simple blood test:
- You’re of Northern European descent (Irish, Scottish, Welsh, Scandinavian)
- You have unexplained fatigue, joint pain, or liver enzyme elevations
- You have type 2 diabetes without obesity or family history
- A close relative (parent, sibling, child) has been diagnosed with hemochromatosis
Genetic testing now costs $150-$300. It’s fast. It’s accurate. And if you test positive, your whole family should be tested too. About 70% of cases are found through family screening after one person is diagnosed.
What About Diet and Supplements?
Yes, diet matters-but not the way you think. You don’t need to stop eating red meat. You don’t need to avoid iron-fortified cereals. The problem isn’t dietary iron-it’s your body’s inability to regulate it.
But here’s what you should avoid:
- Vitamin C supplements with meals (they boost iron absorption)
- Alcohol (it speeds up liver damage)
- Raw shellfish (risk of Vibrio vulnificus infection, which thrives in iron-rich blood)
And if you’re on phlebotomy, don’t take iron supplements. Period. Even if you feel "anemic" after a session, your body isn’t lacking iron-it’s just redistributing it. Taking supplements defeats the whole purpose.
The Future: New Treatments on the Horizon
Phlebotomy works, but it’s not perfect. Some people have bad veins. Others can’t tolerate frequent blood draws. That’s why researchers are testing new drugs.
One promising drug, PTG-300, mimics hepcidin-the hormone your body should be making. In early trials, it reduced transferrin saturation by 53% in 12 weeks. It’s not approved yet, but it could one day replace phlebotomy for some patients.
Another breakthrough? MRI scans can now measure liver iron without a biopsy. The R2* technique gives doctors a precise number-no needles, no risk. That’s huge for monitoring progress.
And scientists are building polygenic risk scores using 27 genetic markers beyond HFE. In trials, they predicted severe iron overload with 89% accuracy. That means we might soon be able to screen people before symptoms even start.
Final Reality Check
Hemochromatosis is not a death sentence. It’s not even a serious illness-if caught early. But it’s deadly if ignored. The same gene mutation that causes iron overload also makes you more likely to develop liver cancer, heart failure, or diabetes later in life.
And here’s the truth: your doctor probably won’t bring it up. Most primary care physicians don’t routinely test transferrin saturation or ferritin for fatigue or joint pain. You have to ask.
If you’re tired all the time, your joints hurt, or you have a family history of liver disease, diabetes, or early heart problems-get tested. A simple blood test can save your life. And if you’re diagnosed? Phlebotomy isn’t a burden. It’s a gift. One that gives you back your energy, your health, and your future.
Can hemochromatosis be cured?
No, hemochromatosis can’t be cured because it’s genetic. But it can be completely managed. With regular phlebotomy, iron levels stay in a safe range, and organ damage stops progressing. People who stick to treatment live normal, healthy lives with no reduced life expectancy.
Is phlebotomy the same as donating blood?
Yes, the process is identical: 450-500 mL of blood is removed. But therapeutic phlebotomy is done for medical reasons, not donation. Blood centers often don’t accept it for transfusion because the patient may have had iron overload, so it’s usually done in a clinic or hospital. The blood is typically discarded unless local regulations allow it to be used.
Why do men get diagnosed more often than women?
Women lose iron naturally through menstruation, pregnancy, and breastfeeding-sometimes for decades. This delays iron buildup. Men don’t have this protective mechanism, so their iron levels rise steadily from their 20s or 30s. By the time women reach menopause, their risk catches up. That’s why many women are diagnosed later in life.
Can I still drink alcohol if I have hemochromatosis?
No. Alcohol increases iron absorption and directly damages liver cells. With hemochromatosis, your liver is already under stress from iron. Adding alcohol is like pouring gasoline on a fire. Even small amounts raise your risk of cirrhosis and liver cancer. Complete abstinence is strongly recommended.
What if I can’t tolerate phlebotomy?
If you can’t handle frequent blood draws-due to low blood pressure, vein issues, or anemia-your doctor may prescribe iron-chelating drugs like deferasirox. These bind to excess iron and help your body remove it through urine or stool. But they’re expensive, have side effects, and are only used when phlebotomy isn’t possible. They’re not a first-line treatment.

Daniel Dover
Got diagnosed last year. Ferritin was 2,100. 42 phlebotomies later, I’m back to hiking. No more brain fog. No more joint pain. It’s not glamorous, but it’s life-changing.