More than 900,000 people worldwide are diagnosed with liver cancer each year, and over 80% of those cases happen in people who already have cirrhosis. This isn’t just a statistic-it’s a reality for millions living with chronic liver disease. If you or someone you care about has cirrhosis, understanding how to catch liver cancer early can mean the difference between living years longer and facing a terminal diagnosis. The good news? Regular screening works. The better news? There are real, effective treatments if cancer is found early. But here’s the problem: most people with cirrhosis never get screened.
Why Cirrhosis Is the Biggest Risk Factor for Liver Cancer
Cirrhosis isn’t just scarring of the liver. It’s a broken repair system. Every time the liver is damaged-by hepatitis B or C, heavy alcohol use, or fatty liver disease-it tries to heal itself. Over time, that healing turns into thick, stiff scar tissue. That scar tissue doesn’t work like healthy liver tissue. And it doesn’t just sit there. It creates the perfect environment for cancer to start growing. Studies show that people with cirrhosis have a 1% to 8% chance each year of developing hepatocellular carcinoma (HCC), the most common type of liver cancer. That risk jumps even higher if you have hepatitis B, especially if it’s not well controlled. People with non-alcoholic fatty liver disease (NAFLD) who’ve developed cirrhosis face a lower but still serious risk-about 1% to 3% per year. The key point? If you have cirrhosis, you’re not just at risk. You’re in the highest-risk group for liver cancer on the planet.How Surveillance Works: The 6-Month Ultrasound Rule
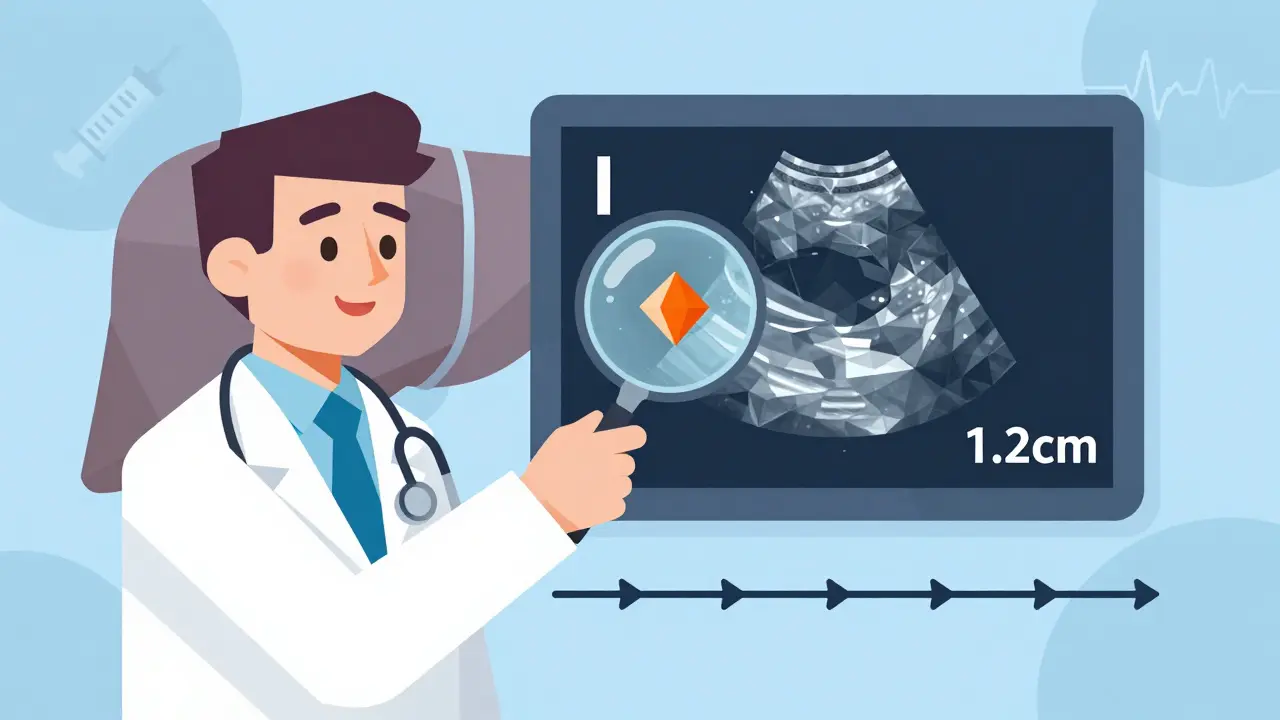
The standard for catching HCC early is simple: get an ultrasound of your liver every six months. That’s it. No fancy scans, no invasive tests. Just a quick, painless, non-radiation imaging test that shows the shape and texture of your liver. Major medical groups-the American Association for the Study of Liver Diseases (AASLD), the European Association for the Study of the Liver (EASL), and others-all agree on this. The reason? HCC tumors grow fast. On average, they double in size every 6 months. If you wait a year for a scan, a tumor that was too small to see could already be the size of a golf ball. But if you scan every 6 months, you’re likely to catch it when it’s still under 2 cm-small enough to be removed or destroyed with high success rates. Some guidelines also suggest adding a blood test for alpha-fetoprotein (AFP), a protein that can rise when liver cancer is present. But AFP isn’t perfect. It can be high for other reasons-like a flare-up of hepatitis-or it can be normal even when cancer is there. So it’s not used alone. It’s a backup. If AFP is above 20 ng/mL (or 20 μg/L), that’s a red flag that needs an immediate follow-up scan.What Happens If Something Shows Up on the Ultrasound?
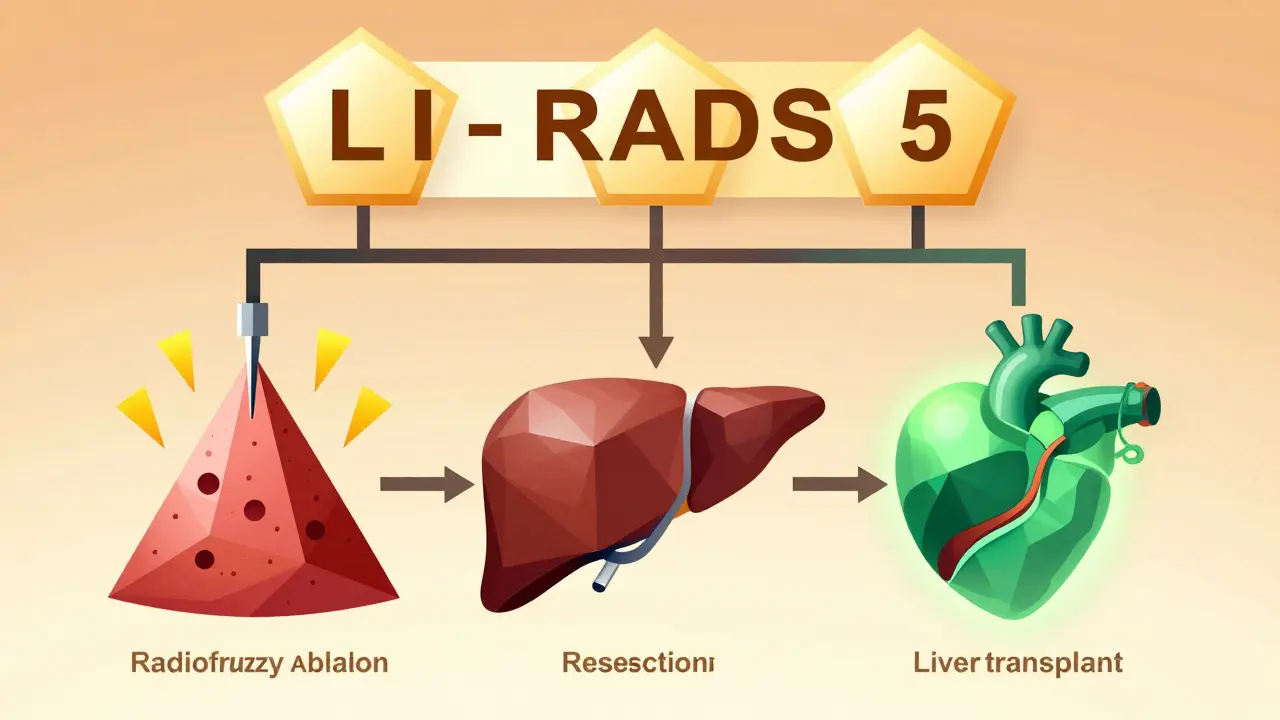
If your 6-month ultrasound finds a lump bigger than 1 cm, the game changes. That’s not a diagnosis yet-it’s a signal. The next step is always a contrast-enhanced CT or MRI scan. These scans use dye to show how blood flows through the liver. Liver cancer has a very specific pattern: it takes up dye quickly on the arterial phase and then loses it fast on the delayed phase. That’s how radiologists tell the difference between a benign nodule and cancer. The Liver Imaging Reporting and Data System (LI-RADS), updated in 2022, gives doctors a clear way to classify what they see. A LI-RADS 5 category means the lesion is almost certainly HCC. A LI-RADS 4 is probably cancer. If you get one of these results, you’re referred to a liver specialist right away.Treatments That Actually Work When Cancer Is Found Early
If HCC is caught at stage 0 or A (small, single tumors under 5 cm, no spread), the chances of long-term survival jump to 50-70%. That’s not a guess. That’s what studies show. Here are the three main treatments that work:- Radiofrequency ablation (RFA): A needle is inserted through the skin into the tumor. High-frequency electrical currents heat and destroy the cancer cells. It’s done as an outpatient procedure, takes under an hour, and has a 90% success rate for tumors under 3 cm.
- Surgical resection: If your liver is healthy enough, surgeons can remove the tumor. This is most common in patients with early cirrhosis (Child-Pugh Class A) and no major complications.
- Liver transplant: For patients with both early HCC and advanced cirrhosis, a transplant removes the cancer and the damaged liver at the same time. The 5-year survival rate after transplant for early HCC is over 70%.
The Big Problem: Most People With Cirrhosis Aren’t Getting Screened
Here’s the hard truth: in the U.S., only about 40% of people with cirrhosis get the recommended 6-month ultrasounds. Why?- Doctors don’t always remember to order the test.
- Patients don’t understand why it matters.
- There’s no automated reminder in most electronic health records.
- Some people can’t afford the time off work or the travel to a specialty center.
New Trends: Risk-Based Screening Is Coming
The old model said: “If you have cirrhosis, you get screened.” The new model says: “Which cirrhotic patients are at highest risk?” The EASL 2023 guidelines introduced risk stratification. They now divide cirrhotic patients into three groups:- High risk (more than 2.5% per year): These patients might get MRI instead of ultrasound, or more frequent scans.
- Medium risk (1.5-2.5% per year): Stick with the standard 6-month ultrasound.
- Low risk (less than 1.5% per year): May not need screening at all.
What You Can Do Right Now
If you have cirrhosis:- Ask your doctor: “Am I on the HCC surveillance list?”
- Confirm your next ultrasound is scheduled for 6 months from your last one.
- Ask if your clinic uses electronic reminders for cirrhosis patients.
- If you’re having trouble getting to appointments, ask about patient navigation services.
- Don’t skip your scans-even if you feel fine. HCC doesn’t cause symptoms until it’s advanced.
What’s Next for HCC Screening and Treatment
The SURVIVE trial, a massive study tracking 10,000 cirrhotic patients, is comparing standard screening to risk-based screening. Results are expected by late 2025. If the data holds, we’ll likely see a shift in U.S. guidelines by 2026. Meanwhile, researchers are testing blood tests that can detect HCC before it shows up on imaging. These “liquid biopsies” look for cancer DNA floating in the bloodstream. If they work, we might one day screen with a simple blood draw every 6 months-no ultrasound needed. For now, though, the best tool is still the 6-month ultrasound. It’s cheap. It’s safe. It’s proven. And it’s underused.FAQ
Do all people with cirrhosis need liver cancer screening?
Yes-if you have cirrhosis, you’re in the highest-risk group for liver cancer. Major guidelines recommend screening for all adults with cirrhosis, unless they’re in the late stage (Child-Pugh Class C) and not eligible for transplant. Even then, some experts still recommend screening if the patient is otherwise stable. The key is: don’t assume you’re safe just because you feel okay. HCC often has no symptoms until it’s too late.
Can a blood test alone detect liver cancer?
No. The AFP blood test is sometimes used alongside ultrasound, but it’s not reliable on its own. About 30-40% of early liver cancers don’t raise AFP levels, and many non-cancer conditions (like hepatitis flare-ups) can raise it. That’s why imaging is required. New biomarker panels like GALAD are promising, but they’re still being tested in large trials and aren’t standard yet.
Is ultrasound safe for liver cancer screening?
Yes. Ultrasound uses sound waves, not radiation. It’s non-invasive, painless, and has no known side effects. It’s the recommended first-line tool because it’s safe enough to do every 6 months for life. Some people feel mild discomfort from the pressure of the probe, but that’s temporary. If you’re anxious about the test, ask your clinic if they offer sedation or if a family member can be with you.
What if I miss a surveillance scan?
Don’t panic, but don’t delay either. Missing one scan doesn’t mean you’re doomed, but it does increase your risk of late diagnosis. Get back on schedule as soon as possible. If it’s been more than 9 months since your last scan, your doctor may recommend an immediate follow-up with a contrast CT or MRI to catch up. Many clinics now use patient navigators to help people reschedule missed appointments-ask if your provider offers this service.
Can lifestyle changes reduce my risk of HCC?
Yes, but not enough to skip screening. Stopping alcohol, losing weight if you have fatty liver, and taking antiviral meds for hepatitis B or C can slow liver damage and lower your cancer risk. But even after hepatitis C is cured, the risk of HCC remains for years if cirrhosis is present. That’s why screening is still required. Lifestyle changes help, but they don’t replace surveillance.
How much does liver cancer screening cost?
In the U.S., a liver ultrasound typically costs between $150 and $300 without insurance. With Medicare or private insurance, it’s often fully covered under preventive care. Adding AFP testing adds $30-$60. Many clinics offer financial assistance for uninsured patients. The cost of missing a scan-especially if cancer is found late-can be tens of thousands of dollars in treatment and lost quality of life. Screening is one of the most cost-effective health actions you can take if you have cirrhosis.

Lisa Davies
Just had my 6-month ultrasound today 🥹 Thank god I didn’t skip it - they found a 1.2cm nodule. Still waiting on the MRI, but I’m already scheduling my transplant eval. This post saved my life. Don’t wait like I did.
PS: My nurse didn’t even mention screening until I asked. Why is this not automatic??