Kava Medication Safety Checker
This tool helps you determine if it's safe to take kava with your current medications and health factors. Based on the article content, kava can cause serious liver damage when combined with certain medications.
Many people turn to kava for anxiety relief, drawn by its reputation as a natural alternative to prescription meds. But here’s the hard truth: if you’re taking any other medication, kava could be putting your liver at serious risk. This isn’t just a warning from a cautious doctor-it’s backed by hospital records, liver transplants, and government health agencies around the world.
What Kava Actually Does to Your Liver
Kava comes from the roots of Piper methysticum, a plant used for centuries in Pacific Island ceremonies. The active ingredients, called kavalactones, help calm the nervous system-similar to how benzodiazepines work, but without the same addiction risk. Sounds good, right? But here’s the catch: kava doesn’t just calm your mind. It also messes with your liver’s ability to process toxins and medications.
Studies show kava depletes glutathione, one of your liver’s main antioxidants. Without enough of it, your liver cells become vulnerable to damage. Worse, kava blocks key liver enzymes-CYP3A4, CYP2C9, and CYP2C19-that break down over 80% of common prescription drugs. When these enzymes are inhibited, medications build up in your system. That’s when things go wrong.
One documented case from UCLA Health involved a patient taking 240 mg of kavalactones daily along with birth control pills, a migraine med, and acetaminophen. Within 17 weeks, their liver enzymes spiked: ALT jumped from under 17 U/L to over 2,400 U/L. Bilirubin hit 40 mg/dL (normal is under 1.2). They needed a liver transplant. This isn’t rare. Between 1984 and 2021, at least 16 cases of kava-induced liver failure were reported in one U.S. county alone. Six of those patients required transplants.
Not All Kava Is the Same
If you’ve ever bought kava powder or capsules, you might not realize how differently it’s made. Traditional Pacific Islanders prepare kava using cold water extraction-grinding the root and mixing it with water. That method has been used safely for thousands of years with almost no reports of liver damage.
But most kava sold in the U.S., Canada, and Europe uses organic solvents like ethanol or acetone to pull out kavalactones faster and more efficiently. These “organic extracts” are the ones linked to liver injury. The FDA’s 2020 review found that 26 out of 26 reported liver toxicity cases in Europe involved these solvent-based products. Water-based kava? Almost none.
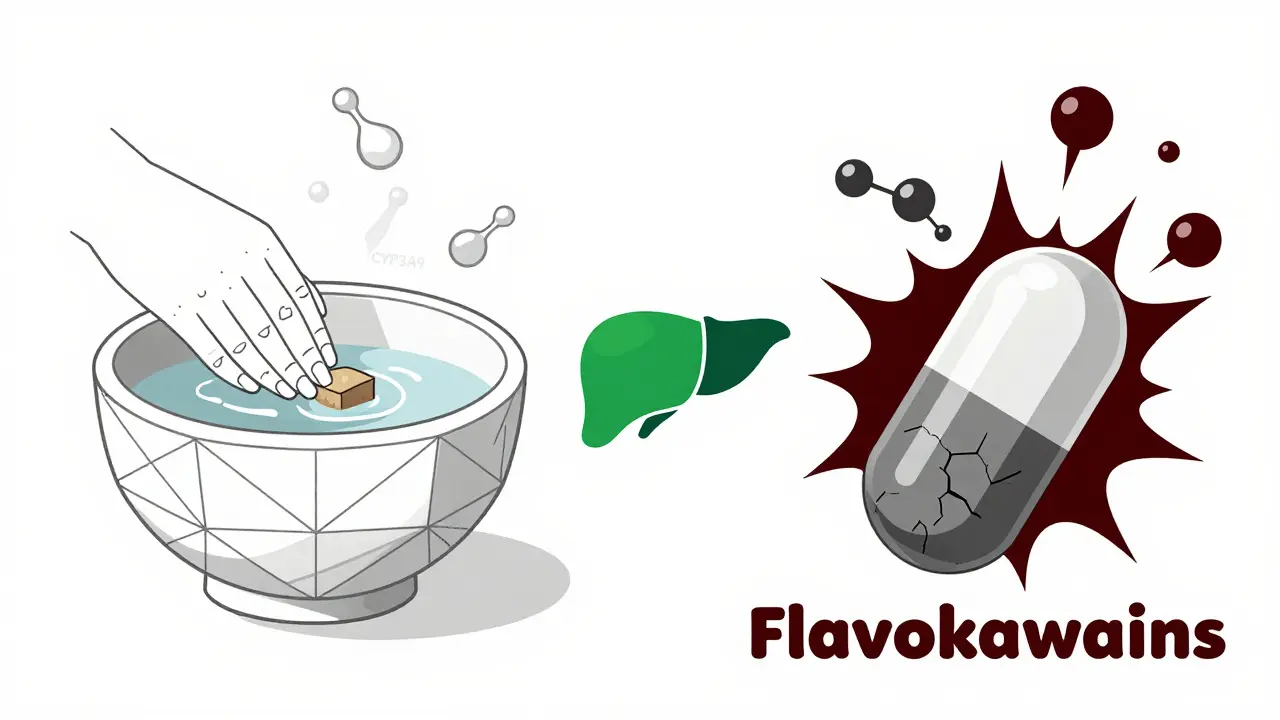
Why does this matter? Because the harmful compounds might not even be the kavalactones. Research now points to flavokawains-chemicals found in higher concentrations in solvent extracts-as the real culprits behind liver damage. So if you’re using a tincture, capsule, or concentrated extract, you’re taking a much bigger risk than someone drinking traditional kava tea.
Medications That Turn Kava Into a Danger Zone
Here’s the list you need to read carefully. If you’re taking any of these, don’t touch kava:
- Acetaminophen (Tylenol) - Even at normal doses, it’s hard on the liver. Combine it with kava, and you’re stacking two liver stressors.
- Benzodiazepines (Xanax, Valium) - Both depress the central nervous system. Together, they can cause extreme drowsiness, slowed breathing, and overdose.
- Antidepressants (SSRIs, SNRIs) - Many are metabolized by CYP enzymes kava blocks. This raises drug levels and increases side effects like serotonin syndrome.
- Statins (Lipitor, Crestor) - These cholesterol drugs are already linked to rare liver issues. Kava can push them over the edge.
- Antibiotics (like erythromycin) - Some are processed by the same liver enzymes kava shuts down.
- Anticoagulants (Warfarin) - Kava can interfere with clotting, raising bleeding risk.
- Birth control pills - Hormonal meds are metabolized by CYP3A4. Kava slows their breakdown, increasing estrogen levels and liver strain.
- Anti-seizure drugs - Valproate and carbamazepine are both hepatotoxic. Add kava? High risk of liver failure.
The American Association for the Study of Liver Diseases (AASLD) says clearly: if you’re on any medication processed by CYP3A4, CYP2C9, or CYP2C19, avoid kava. That covers a huge chunk of prescriptions.
Who’s Most at Risk?
It’s not just about what you’re taking. Your body matters too. Four factors make liver damage from kava much more likely:
- Pre-existing liver disease - Even mild fatty liver or hepatitis increases vulnerability.
- Heavy alcohol use - Alcohol already stresses the liver. Kava adds another layer of damage.
- High doses - Taking more than 250 mg of kavalactones daily is linked to higher risk. Most supplements contain 60-280 mg. Going over that is playing with fire.
- Genetic differences - Some people naturally have slower versions of liver enzymes. If you’re one of them, even normal kava doses can be dangerous.
One woman in her 40s, healthy and active, took kava capsules for anxiety and a low-dose statin. Within three months, her ALT jumped from 28 to 320. She stopped kava immediately. Her enzymes returned to normal in six weeks. But she was lucky. Others aren’t.
What to Do If You’re Already Using Kava
If you’re taking kava and any medication, stop immediately. Don’t wait for symptoms. Liver damage from kava often shows up late-when it’s already severe.
Look for early signs:
- Unexplained fatigue
- Dark urine
- Yellowing of skin or eyes (jaundice)
- Abdominal pain, especially on the right side
- Nausea or vomiting without reason
Go to your doctor and ask for a liver panel: ALT, AST, bilirubin, and ALP. If your ALT is over 50 U/L and you’re using kava, that’s a red flag. In one case, a Reddit user didn’t realize kava was the problem until their ALT hit 300. Their doctor had to ask-because the patient never mentioned taking supplements.
Don’t assume your doctor knows about kava. Most aren’t trained in herbal interactions. Bring printed info from the FDA or WHO. Say: “I’m taking kava. Can we check my liver enzymes?”

Alternatives to Kava for Anxiety
If you’re using kava for anxiety, you don’t have to go back to prescription pills. There are safer options:
- Valerian root - Shown in clinical trials to help with sleep and mild anxiety, with no known liver toxicity.
- L-theanine - An amino acid in green tea that promotes calm without drowsiness. Works well with magnesium.
- Magnesium glycinate - Deficiency is linked to anxiety. Supplementing can help, especially if you’re stressed or sleep-deprived.
- Cognitive behavioral therapy (CBT) - Proven to be as effective as medication for anxiety, with zero side effects.
- Regular exercise - Just 30 minutes of walking five days a week reduces anxiety as effectively as SSRIs in some studies.
None of these carry the same risk profile as kava. And none require a liver test before you start.
Why This Isn’t Just a ‘Natural vs. Synthetic’ Issue
Some people say, “It’s natural, so it’s safe.” That’s a dangerous myth. Kava isn’t like chamomile tea. It’s a potent biochemical agent that interacts with your body’s core systems. The fact that it’s sold as a supplement doesn’t mean it’s harmless. Supplements aren’t tested like drugs. They don’t have to prove safety before hitting shelves.
Compare this to prescription anxiolytics. If a drug caused 11 liver transplants in the U.S. alone, it would be pulled from the market overnight. Kava? Still on shelves. Why? Because it’s a plant. But plants can be deadly. Digitalis from foxglove kills. Kava can, too.
The real issue isn’t natural versus synthetic. It’s whether something is safe for your body-especially when you’re already taking other meds. And the data says: kava, especially in extract form, is not safe if you’re on medication.
Final Advice: When in Doubt, Skip It
If you’re taking any prescription or over-the-counter medication, don’t risk it. Kava’s benefits for anxiety are modest at best. The risk of liver failure is real, documented, and preventable.
Even if you’re healthy, not on meds, and using water-based kava-still be cautious. Limit use to no more than 4 weeks at a time. Take breaks. Get liver tests if you use it regularly.
And if you’re a healthcare provider? Always ask about supplements. Patients rarely volunteer that info. One study found that 80% of patients with kava-induced liver injury had never told their doctor they were taking it.
Your liver doesn’t scream until it’s too late. Don’t wait for it to cry out.
Can I take kava with my anxiety medication?
No. Combining kava with anxiety medications like benzodiazepines, SSRIs, or SNRIs significantly increases the risk of liver damage and dangerous sedation. Kava inhibits liver enzymes that break down these drugs, causing them to build up in your system. This can lead to overdose, liver failure, or even death. If you’re on anxiety meds, avoid kava entirely.
Is water-based kava safer than capsules or tinctures?
Yes. Traditional water-based kava preparations, used for centuries in the Pacific Islands, have very few documented cases of liver injury. In contrast, organic solvent extracts (ethanol or acetone-based) found in capsules, tinctures, and concentrates are strongly linked to liver toxicity. These extracts contain higher levels of flavokawains, which appear to be the main cause of liver damage. Stick to traditional preparations if you choose to use kava at all.
How long does it take for kava to damage the liver?
Liver damage can develop as early as 4-8 weeks of regular use, but in many documented cases, symptoms appear after 12-17 weeks. One patient developed jaundice at 16 weeks and required a liver transplant by week 17. There’s no safe timeline-some people react quickly, others take longer. The risk increases with higher doses, longer use, and combining kava with other medications or alcohol.
Should I get my liver tested if I’ve taken kava?
Yes-if you’ve taken kava within the past 6 months, especially if you’re on other medications. Get a liver panel (ALT, AST, bilirubin, ALP). Normal results don’t guarantee safety, but elevated enzymes are a clear warning. If your ALT is over 50 U/L and you’ve used kava, stop immediately and consult a doctor. Many cases of kava-induced liver injury are reversible if caught early.
Why is kava still sold if it’s dangerous?
In the U.S., kava is classified as a dietary supplement, not a drug. That means it doesn’t need FDA approval before being sold. While the FDA has issued warnings since 2002, it can’t ban it without overwhelming evidence of harm-something the supplement industry fights hard against. Other countries like Australia, Canada, and most of Europe have banned or restricted kava due to liver risks. The fact that it’s still available doesn’t mean it’s safe.


Steven Destiny
Kava is a trap disguised as a remedy. I used it for months thinking I was being ‘natural’-until my ALT hit 412. My doctor looked at me like I’d been drinking paint thinner. No more kava. Ever. If you’re on meds, just say no. Your liver didn’t sign up for this.