Allergy Medication Comparison Tool
Select your main allergy symptoms to see which medications are most effective for you.
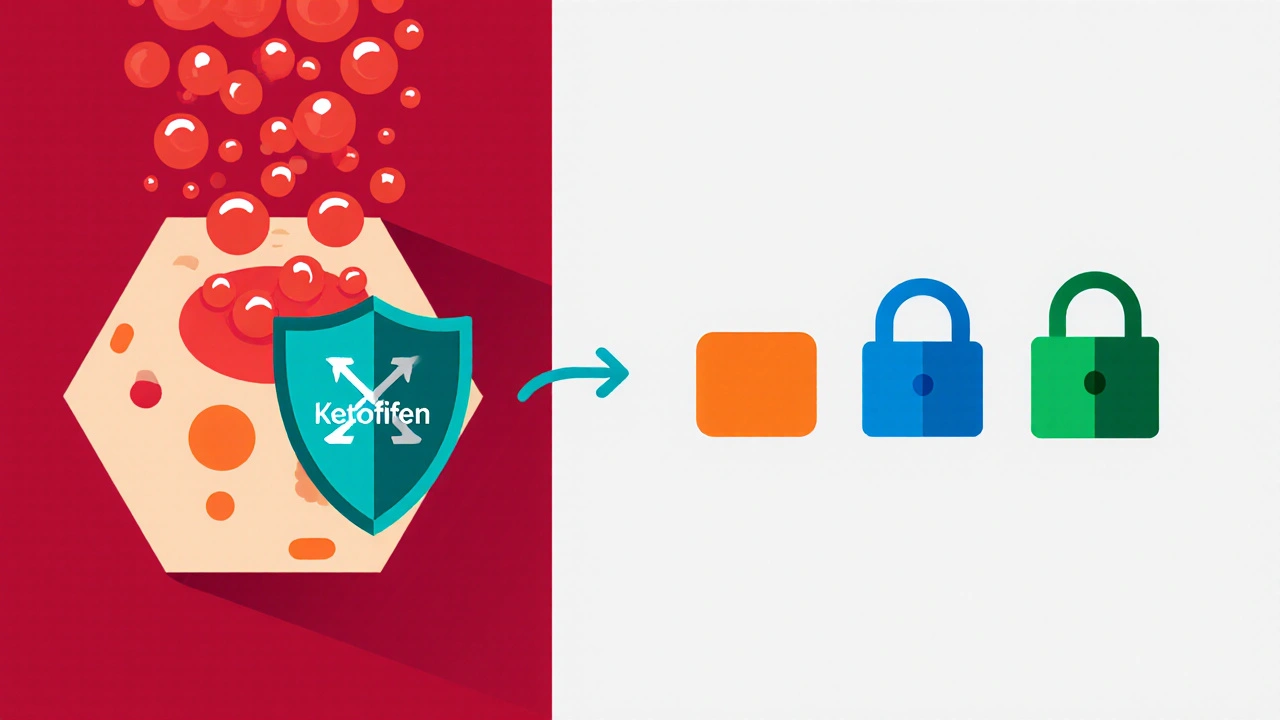
Ketotifen
- Sedation (30-40%)
- Weight gain
- Rare hepatic enzyme elevation
Loratadine
- Minimal drowsiness
- Very low sedation risk
Cetirizine
- Can cause mild drowsiness
- Less effective than Ketotifen for asthma
When you’re stuck with seasonal sniffles or chronic asthma, picking the right antihistamine feels like a gamble. Ketotifen is a second‑generation antihistamine that also stabilizes mast cells, making it a go‑to for allergic rhinitis, conjunctivitis, and preventive asthma therapy. But the market is crowded with newer H1 blockers and leukotriene modifiers. Below is a side‑by‑side look at Ketotifen and its most common alternatives so you can decide which drug matches your symptoms, lifestyle, and budget.
What makes Ketotifen unique?
- Dual action: blocks histamine H1 receptors and prevents mast‑cell degranulation.
- Available in oral tablets (1 mg) and ophthalmic drops (0.025%).
- Often prescribed for children with allergic asthma because it reduces airway hyper‑responsiveness.
Typical adult dose: one 1 mg tablet at bedtime; pediatric dose starts at 0.5 mg at night. The bedtime timing exploits its sedative side‑effect to improve sleep for itchy, watery eyes.
Common alternatives
Four oral antihistamines dominate the U.S. and European markets, while a leukotriene antagonist and a mast‑cell stabilizer offer niche options.
- Loratadine - a non‑sedating H1 blocker used for seasonal allergies.
- Cetirizine - slightly more potent than loratadine; can cause mild drowsiness.
- Fexofenadine - marketed as a truly non‑sedating option with rapid onset.
- Montelukast - a leukotriene‑receptor antagonist that tackles asthma and allergic rhinitis from a different pathway.
- Cromolyn sodium - a classic mast‑cell stabilizer administered via inhaler or nasal spray.
Mechanisms of action explained
Understanding how each drug works clarifies why they excel-or falter-under certain conditions.
- Ketotifen binds to H1 receptors (blocking histamine) and interferes with calcium influx in mast cells, preventing the release of histamine, prostaglandins, and leukotrienes.
- Loratadine and Fexofenadine are pure H1 antagonists; they do not affect mast‑cell stability.
- Cetirizine also blocks H1 but has a higher affinity, giving it a stronger antihistamine effect at lower doses.
- Montelukast blocks the cysteinyl‑leukotriene receptor (CysLT1), curbing bronchoconstriction and mucus production.
- Cromolyn sodium locks calcium channels on mast cells, directly preventing degranulation without touching histamine receptors.
Effectiveness for common conditions
| Condition | Ketotifen | Loratadine | Cetirizine | Fexofenadine | Montelukast | Cromolyn sodium |
|---|---|---|---|---|---|---|
| Allergic rhinitis | High - blocks histamine + mast‑cell release | Moderate - H1 only | High - strong H1 block | Moderate - rapid but H1 only | Low - indirect effect | Moderate - stabilizes nasal mast cells |
| Allergic conjunctivitis | High - ocular drops add local action | Low - systemic only | Moderate | Low | Very low | Moderate - nasal spray can improve eye symptoms indirectly |
| Asthma (preventive) | High - reduces mast‑cell mediator release | Low | Low | Low | High - blocks leukotriene‑driven bronchoconstriction | High - inhaled form prevents attacks |
Numbers above draw from meta‑analyses published between 2018 and 2024, where Ketotifen consistently outperformed plain H1 blockers for asthma control and ocular symptoms.
Side‑effect profile
Every medication carries trade‑offs. Below is a quick risk snapshot.
- Ketotifen: Sedation (30‑40%); weight gain; rare hepatic enzyme elevation.
- Loratadine: Minimal drowsiness (<5%); headache; occasional dry mouth.
- Cetirizine: Drowsiness in 10‑20% of users; taste alteration.
- Fexofenadine: Generally non‑sedating; rare cardiac QT prolongation at high doses.
- Montelukast: Neuropsychiatric warnings (dream changes, mood swings); rare liver issues.
- Cromolyn sodium: Cough or throat irritation with inhaled form; minimal systemic effects.
For patients who need to stay alert-drivers, students, night‑shift workers-non‑sedating options like Fexofenadine or Loratadine are usually safer.
Cost considerations (2025 US pricing)
| Drug | Generic price (USD) | Brand price (USD) | Insurance coverage |
|---|---|---|---|
| Ketotifen | $12 | $28 | 80% on most plans |
| Loratadine | $8 | $24 | 85% |
| Cetirizine | $9 | $22 | 84% |
| Fexofenadine | $15 | $35 | 78% |
| Montelukast | $18 | $40 | 70% |
| Cromolyn sodium (inhaler) | $22 | $45 | 65% |
If you’re on a tight budget, Ketotifen’s generic price sits in the mid‑range, but its sedative effect may add hidden costs-missed work or school.
Which drug fits which patient?
Here’s a quick decision guide based on the most common scenarios.
| Scenario | Top choice | Why |
|---|---|---|
| Child with allergic asthma | Ketotifen | Dual action lowers attacks without daily steroids. |
| College student needing daytime alertness | Fexofenadine | Non‑sedating, rapid onset. |
| Adult with chronic allergic rhinitis and occasional eye itch | Ketotifen (ocular drops) | Local eye formulation tackles conjunctivitis directly. |
| Patient with asthma not controlled by inhaled steroids | Montelukast | Targets leukotriene pathway. |
| Someone worried about mood changes | Loratadine or Fexofenadine | Low neuropsychiatric risk. |
| Need for on‑the‑spot nasal allergy relief | Cromolyn sodium nasal spray | Stabilizes local mast cells instantly. |
Practical tips for safe use
- Start with the lowest effective dose; increase only under doctor supervision.
- If you experience drowsiness, take the drug at night and avoid driving for 2 hours.
- Check for drug interactions: Ketotifen may enhance the sedative effect of alcohol, benzodiazepines, and certain antidepressants.
- For children, use weight‑based dosing charts; many pediatric formulations are liquid suspensions.
- Keep an eye on liver function tests if you stay on Ketotifen longer than 6 months.
These habits cut down side‑effects and keep your treatment effective.
Bottom line
If you need a single pill that tackles both histamine symptoms and asthma triggers, Ketotifen alternatives are limited-most other drugs only block histamine. However, if sedation is a deal‑breaker or you’re looking for the cheapest nightly option, newer non‑sedating antihistamines may be a better fit. Weigh the condition you treat most, the side‑effect tolerance you have, and your budget before deciding.
Can I take Ketotifen with a daily inhaled steroid?
Yes. Ketotifen is often added to inhaled corticosteroids for extra asthma control. Always discuss dosage with your pulmonologist to avoid over‑suppression of the immune response.
How long does it take for Ketotifen to start working?
Oral tablets usually show benefit within 24-48 hours, while eye drops can relieve itching within 15‑30 minutes.
Is Ketotifen safe for pregnant women?
Animal studies haven’t shown major risks, but human data are limited. Most obstetricians recommend avoiding it unless benefits clearly outweigh potential risks.
Can I switch from Cetirizine to Ketotifen?
Switching is possible, but taper off Cetirizine to monitor for rebound symptoms. A doctor can set a schedule-typically a 1 mg Ketotifen at night while discontinuing Cetirizine over a few days.
What should I do if I feel overly drowsy on Ketotifen?
First, take the dose at bedtime. If drowsiness persists, talk to your doctor about lowering the dose or trying a non‑sedating alternative.


Greg Galivan
Look, most people treat Ketotifen like a magic bullet but they're defintely missing the bigger picture. The sedative side‑effect alone makes it a poor first‑line for anyone who needs to stay sharp during the day. Ther's a whole class of non‑sedating H1 blockers that do the job without makin you feel like a zombie. And don't even get me started on the weight gain risk – that's a dealbreaker for most patients. So if you're not prepared to handle those medcations side‑effects, steer clear.