What if your meds worked better-and hurt less-just by changing how you live?
You’re taking your blood pressure pill every morning. Your diabetes meds are on schedule. Your antidepressant? Taken like clockwork. But you’re still tired, bloated, nauseous, or achy. You might think it’s just the price of staying healthy. But what if those side effects aren’t inevitable? What if they’re partly caused by things you eat, how you move, or how you sleep?
Here’s the truth: lifestyle changes aren’t just helpful-they’re powerful tools that can cut medication side effects in half for many people. And it’s not magic. It’s science. A 2021 study in JAMA Internal Medicine found that side effects from medications send nearly 7 out of every 100 hospital patients through the door. Many of those cases weren’t due to bad drugs-they were due to bad habits clashing with those drugs.
You don’t need to quit your meds. You don’t need to overhaul your life overnight. But if you tweak a few daily routines, you could feel better, need lower doses, and avoid trips to the ER. This isn’t theory. It’s what’s happening in clinics right now-from Melbourne to Minneapolis.
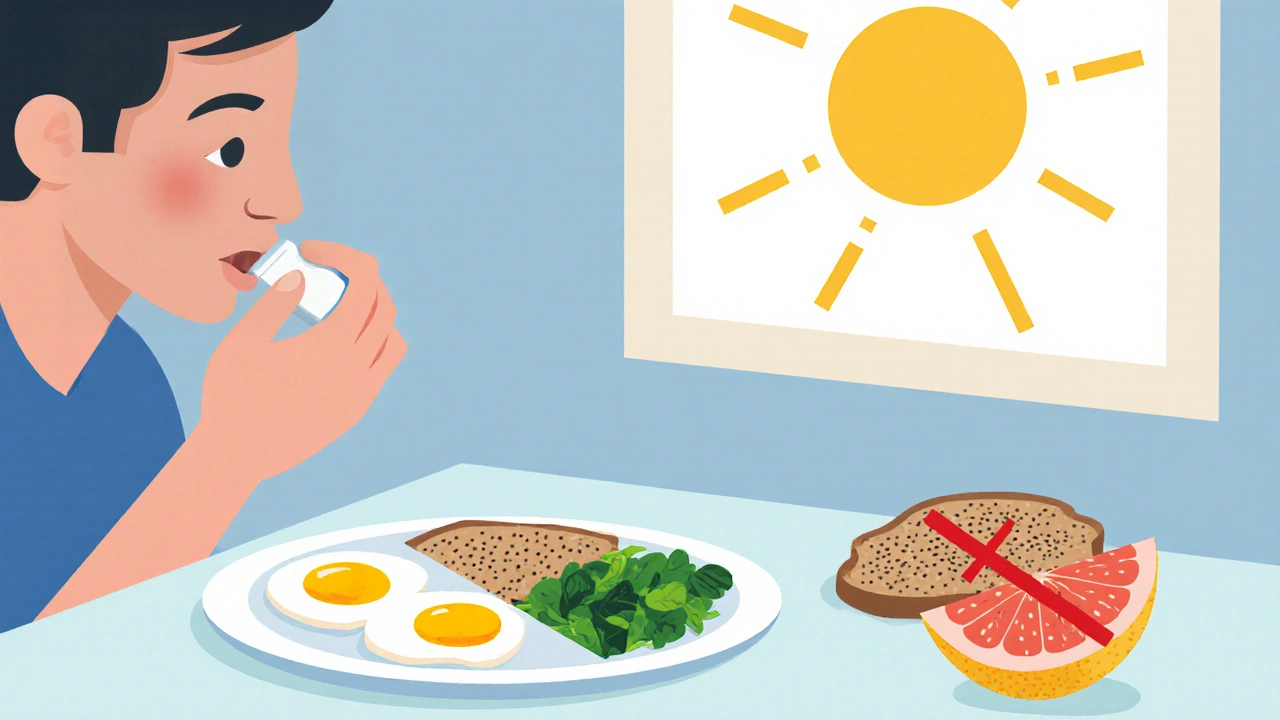
How your diet can make or break your meds
Food isn’t just fuel. It’s a co-pilot for your meds. Some foods boost them. Others block them. And some turn them into trouble.
Take warfarin, a blood thinner. If you suddenly start eating a big bowl of kale or spinach every day-rich in vitamin K-you’re undoing the drug’s effect. That’s not a myth. Studies show vitamin K can cut warfarin’s effectiveness by 30-50%. The fix? Keep your intake steady. Don’t go from zero greens to three cups a day. Just pick a consistent amount and stick with it.
Then there’s grapefruit juice. One glass a day can turn your statin-meant to lower cholesterol-into an overdose. It blocks an enzyme in your liver (CYP3A4) that normally breaks down the drug. Blood levels spike by 15-50%. That raises your risk of muscle damage. If you take simvastatin, atorvastatin, or lovastatin, skip the grapefruit. Orange juice? Fine. But grapefruit? No.
For diabetes meds like metformin, stomach upset is common. But a 2022 study in Diabetes Care found that people who ate the same amount of carbs at each meal-about 30 grams-cut their nausea and diarrhea by 37%. That means no huge pasta dinners followed by a protein bar at midnight. Stick to balanced meals. Spread carbs out. Your gut will thank you.
And if you’re on a GLP-1 agonist like semaglutide (Ozempic, Wegovy), nausea hits 73% of people early on. The fix? Eat slowly. Chew each bite 20-30 times. Keep meals under 500 calories. Avoid spicy, greasy, or acidic foods. And don’t eat within three hours of bedtime. These small shifts cut nausea down to 29%.
Move more-even if you’re tired
Feeling sluggish on beta-blockers? That’s common. But research from the American Heart Association shows that starting with just 10 minutes of walking twice a day, then building up to 30 minutes five days a week, improves energy levels by 41% in eight weeks.
It’s not about running marathons. It’s about moving consistently. For statin users with muscle pain, a 2021 study in the Journal of the American College of Cardiology found that adding light resistance training-two sets of 10 reps, twice a week-cut muscle pain from 29% to 11%. Pair that with 200mg of coenzyme Q10 daily, and the results get even better.
And if you’re on antidepressants? Weight gain is a real concern. On average, people gain 7.3 pounds in the first year. But when they added 150 minutes of moderate exercise (like brisk walking or cycling) each week-plus protein-rich meals (1.6g per kg of body weight)-they cut that gain by two-thirds. That’s not just about looking better. It’s about keeping your metabolism stable and your meds working right.
Sleep isn’t just rest-it’s medicine
Most people don’t realize their liver works overtime while they sleep. That’s when your body processes most meds. If you’re sleeping less than 7 hours, or your sleep is broken, your liver enzymes don’t do their job well. That means drugs stick around longer-or don’t break down enough.
A National Sleep Foundation study found that people who got 7-9 hours of quality sleep (measured by sleep trackers) metabolized drugs like statins and some antidepressants 22% more efficiently. That means fewer side effects and more stable levels.
Fixing sleep isn’t about fancy gadgets. It’s about consistency. Go to bed and wake up at the same time-even on weekends. No screens an hour before bed. Keep your room cool and dark. If you’re on a med that makes you drowsy, take it at night. If it keeps you awake, take it in the morning. Timing matters.
Stress is a silent drug interaction
Chronic stress raises cortisol. High cortisol messes with your blood sugar, your immune system, and how your body handles meds. For people on antidepressants, stress can make them less effective. A 2021 JAMA Psychiatry study showed that 30 minutes of daily mindfulness-just sitting quietly, focusing on your breath-lowered cortisol by 27% and boosted antidepressant effectiveness by 31%.
You don’t need a meditation app or a yoga mat. Try this: Set a timer for 10 minutes, twice a day. Sit in a chair. Close your eyes. Breathe in for four counts. Hold for four. Breathe out for six. That’s it. Do it after breakfast and before dinner. After eight weeks, most people notice they feel calmer, sleep better, and their meds work smoother.
Alcohol, smoking, and meds: a bad combo
Alcohol and antidepressants? Dangerous. It can make you more drowsy, increase liver damage risk, and worsen depression. Even one drink a day can interfere. If you’re on metronidazole, any alcohol can cause vomiting, flushing, and a racing heart. Don’t risk it.
Smoking? It speeds up how your body breaks down some meds. If you smoke and take clozapine (for schizophrenia), your dose might need to be higher. Quitting smoking can cause side effects to return if your dose isn’t adjusted. Always tell your doctor if you start or stop smoking.
What your doctor should ask you (but probably doesn’t)
Most doctors focus on your labs and symptoms. But they rarely ask: “How are you sleeping?” “What does your typical day of eating look like?” “Do you drink alcohol?” “How much do you move?”
A 2023 survey found only 38% of primary care visits included any structured check on lifestyle habits-even though 76% of patients take two or more meds with known lifestyle interactions.
Here’s what you can do: Before your next appointment, write down answers to these six questions:
- How many minutes of movement do I get each day? (Walking counts.)
- What does my typical breakfast, lunch, and dinner look like?
- Do I eat the same amount of greens or grapefruit every day?
- How many hours do I sleep? Do I wake up feeling rested?
- Do I drink alcohol? How much?
- Do I feel stressed most days? What helps me calm down?
Bring this list. Ask: “Could any of this be making my side effects worse?” Most doctors will be glad you asked.

Real results from real programs
Cleveland Clinic’s Lifestyle 180 program helped people with high blood pressure, diabetes, and high cholesterol cut their meds by 72% over six months. How? Four simple rules:
- 45 minutes of daily walking or cycling
- Mediterranean diet with less than 50g of added sugar per day
- 7.5 hours of sleep, tracked with a wearable
- Two 10-minute mindfulness sessions daily
Patients didn’t just feel better-they needed fewer pills. Same story in North Carolina’s Medication Optimization Program: after 12 weeks of weekly coaching, people reduced side effects by 50% and improved adherence by 40%.
What not to do
Don’t stop your meds because you feel better. Don’t cut your dose because you started walking. Don’t start taking coenzyme Q10 or magnesium just because you read about it online.
All changes must happen under medical supervision. Stopping blood pressure meds suddenly can cause a dangerous spike. Skipping insulin can lead to diabetic ketoacidosis. Lifestyle changes work best when they’re paired with your doctor’s plan-not replace it.
Also, don’t wait for your doctor to bring it up. You’re the expert on your life. If you’re struggling with side effects, speak up. Bring data. Bring your habits. Bring your questions.
Start small. Stay consistent.
You don’t need to fix everything at once. Pick one thing. Maybe it’s swapping your morning donut for an egg and spinach. Maybe it’s walking for 10 minutes after dinner. Maybe it’s turning off your phone an hour before bed.
Do that for two weeks. Then add one more. In three months, you won’t just be managing side effects-you’ll be taking control.
Your meds are tools. But your lifestyle? That’s the foundation. Build it right, and you won’t just survive your treatment-you’ll thrive through it.
Can lifestyle changes really reduce the need for medication?
Yes, in many cases. Studies show that consistent lifestyle changes-like regular exercise, better sleep, and balanced eating-can lower blood pressure, improve blood sugar control, and reduce cholesterol enough that doctors may reduce doses. For example, 30-40% of people on blood pressure meds can lower their dose after adopting the DASH diet and 150 minutes of weekly walking. But this only happens under medical supervision. Never stop or lower your meds without talking to your doctor.
What foods should I avoid with my meds?
It depends on your meds. Grapefruit juice can dangerously increase levels of statins and some blood pressure drugs. Vitamin K-rich foods like kale and spinach can reduce the effect of warfarin. Alcohol can worsen drowsiness from antidepressants or cause dangerous reactions with metronidazole. Always ask your pharmacist for a list of food-drug interactions specific to your prescriptions.
I’m tired all the time on my meds. Can exercise help?
Yes-even if you feel too tired to move. Fatigue from beta-blockers or antidepressants often improves with gentle, consistent movement. Start with 10 minutes of walking twice a day. After 4-6 weeks, most people report a 40% increase in energy. Exercise doesn’t drain you-it helps your body use energy more efficiently.
How long does it take for lifestyle changes to reduce side effects?
Some changes, like better sleep or cutting grapefruit juice, can show results in days. Others, like improved fitness or weight management, take 6-12 weeks. Programs like Cleveland Clinic’s Lifestyle 180 show measurable results in 8-12 weeks. Patience and consistency matter more than speed.
Should I take supplements like CoQ10 to reduce statin side effects?
Some studies show that 200mg of CoQ10 daily, combined with light strength training, reduces statin-related muscle pain. But supplements aren’t regulated like drugs. Talk to your doctor first. They can check for interactions and recommend a reliable brand. Don’t self-prescribe.
Can stress make my meds less effective?
Absolutely. High stress raises cortisol, which interferes with how your body processes antidepressants, diabetes meds, and even thyroid hormones. A 2021 study found that 30 minutes of daily mindfulness improved antidepressant effectiveness by 31%. Managing stress isn’t optional-it’s part of your treatment plan.
What’s next?
If you’re taking two or more meds, your next step is simple: write down your top three side effects. Then, pick one lifestyle habit that might be making them worse. Change that one thing for two weeks. Track how you feel. Then talk to your doctor. You’re not just a patient-you’re the CEO of your health. And you’ve got more power than you think.

Will RD
I tried this stuff. Didn't work. Now I'm on 7 meds and still feel like garbage. 🤷♂️