Acute vs. Chronic Low Back Pain: It’s Not Just About How Long It Hurts
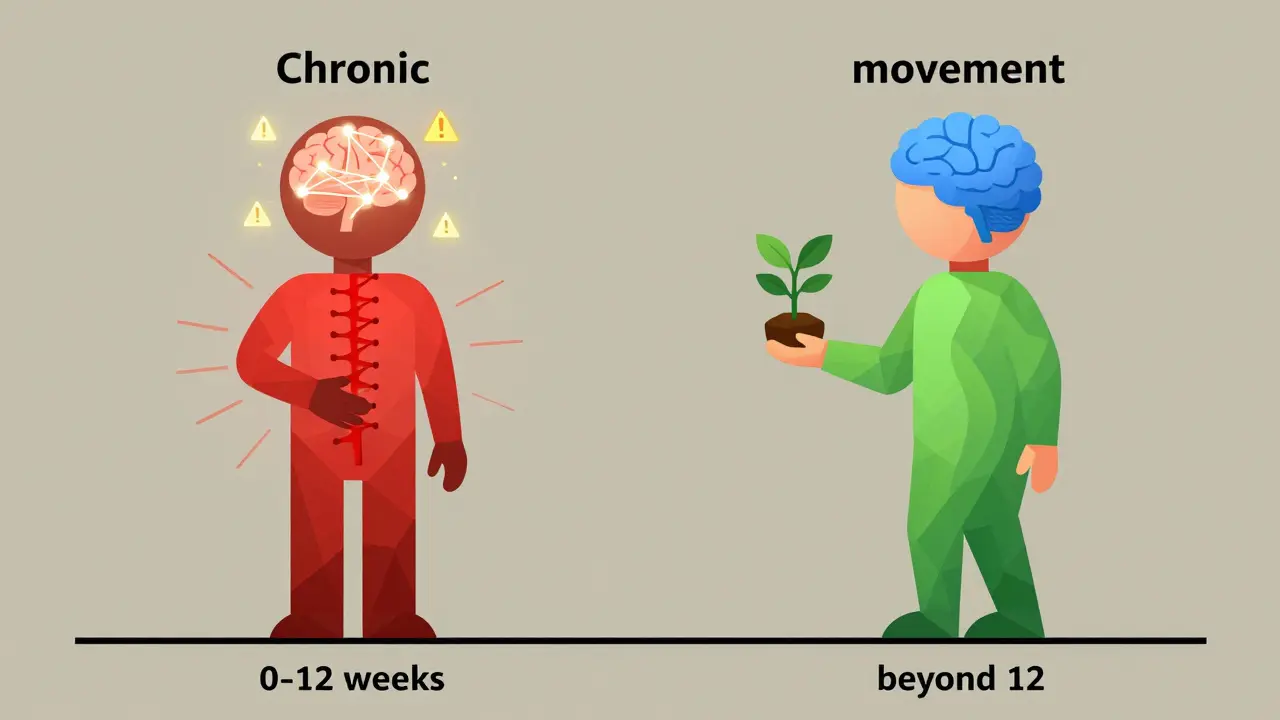
If you’ve ever thrown out your back lifting groceries or twisted wrong getting out of bed, you know how sharp and scary that pain can be. But if you’ve been dealing with it for months-or years-you also know it’s a totally different beast. The difference between acute and chronic low back pain isn’t just how long it lasts. It’s about what’s happening inside your nervous system, how your body responds, and most importantly, how you should treat it.
Acute low back pain hits fast and hard. It usually starts after a clear injury: lifting something heavy, slipping on ice, or even coughing too hard. Most people feel it as a sudden, localized ache or sharp stab. It’s the kind of pain that makes you freeze mid-step. But here’s the good news: about 90% of these cases clear up on their own within 4 to 12 weeks. That’s the body healing a strained muscle or irritated ligament. No surgery. No pills. Just time and smart movement.
Chronic low back pain is different. It doesn’t always have a clear starting point. Sometimes it begins after an acute injury that never fully healed. Other times, it just shows up-no trauma, no accident. The pain lingers past the three-month mark, often stretching into years. The tissues may be fine, but your nervous system isn’t. Your brain and spinal cord have become hypersensitive. Even a light touch or a normal movement can trigger pain signals. This isn’t weakness. It’s biology. And it’s why simply stretching or massaging won’t fix it.
Why Timing Matters More Than You Think
One of the biggest mistakes people make is waiting. If you’re in pain for more than a week, you might think, "I’ll just rest it for a few days." But rest too long, and you’re setting yourself up for a longer fight. Research shows that starting physical therapy within 72 hours of acute pain onset cuts your risk of turning chronic by 22%. That’s not a small number. That’s life-changing.
Why? Because movement is medicine-not just for healing tissue, but for training your nervous system. When you stay still, your brain starts to associate movement with danger. Your muscles tighten. Your posture shifts. Your fear grows. That’s the beginning of a feedback loop that turns short-term pain into long-term suffering.
Physical therapy for acute back pain isn’t about deep tissue massage or fancy machines. It’s about relearning how to move safely. A good therapist will teach you how to bend, lift, and stand without triggering pain. They’ll use simple exercises to restore normal movement patterns. Studies show that people who start PT early see a 40-60% drop in pain intensity and cut their time off work by nearly half. And crucially, 84% of them avoid chronic pain altogether.
But if you wait too long-say, beyond 16 days-the odds flip. Your risk of chronic pain jumps by 38%. That’s not a coincidence. That’s science. Your nervous system is rewiring itself. The window to stop it is narrow. Miss it, and you’re playing defense instead of offense.
What Physical Therapy Actually Does for Chronic Pain
When pain sticks around past six months, the rules change. You can’t just "fix" the back. You have to retrain the brain. That’s where pain neuroscience education comes in. It’s not a buzzword. It’s a proven method.
Most people with chronic back pain believe their pain means damage. "My spine is worn out," they say. "My discs are bulging. I need surgery." But MRI scans often show the same changes in people with zero pain. The problem isn’t the structure-it’s the signal. Your nervous system is screaming when it shouldn’t be.
Good physical therapy for chronic pain starts with education. Your therapist explains how pain works-not just in your back, but in your nerves, your brain, your stress response. They help you understand that pain doesn’t equal damage. That’s a game-changer. People who get this message are 71% more likely to report meaningful improvement.
Then comes graded exposure. Instead of avoiding movement because it hurts, you slowly, safely do more. You start with small steps: walking 5 minutes, then 10. Sitting for 15 minutes, then 20. Lifting a light bag, then a heavier one. Each success tells your brain: "This isn’t dangerous." Over time, the pain fades-not because the tissue healed, but because your nervous system learned to trust again.
Real results? About 30-50% of people with chronic pain see a meaningful drop in pain levels. Around 60-70% improve their ability to move, work, and sleep. Complete pain relief? Rare. But functional recovery? Very possible. And that’s the real goal: living well, even if you still feel some discomfort.
What Doesn’t Work (And What Does)
Let’s be clear: not all physical therapy is created equal.
For acute pain, the most effective approach is mechanical diagnosis and movement therapy. That means your therapist watches how you move, finds the pattern that triggers pain, and teaches you how to correct it. Think: learning to squat without arching your back, or standing up from a chair without jolting your spine. This works because it’s targeted. It’s not random exercises. It’s solving a specific movement problem.
For chronic pain, the same approach falls short. You need something deeper. That’s where pain neuroscience education becomes essential. Studies show therapists with certification in this area get 82% better outcomes. Why? Because they don’t just treat the body. They treat the fear, the anxiety, the belief that pain means you’re broken.
What doesn’t work? Long-term rest. Overuse of imaging (like MRIs) for acute pain. Excessive medication. And therapy that’s just stretching and heat packs without a plan. A 2022 study found that over-medicalizing acute pain-sending people for scans and specialist referrals too early-actually increased chronicity risk by 27%. Sometimes, doing nothing (the right nothing) is better than doing too much.
And don’t fall for the "miracle cure" claims. There’s no magic brace, no miracle supplement, no laser that fixes chronic back pain overnight. Real progress is slow, consistent, and built on understanding-not quick fixes.
What to Expect From Treatment
If you’re dealing with acute pain, expect 6 to 12 sessions over 3 to 6 weeks. The first few visits focus on reducing pain through gentle movement, ice or heat, and learning how to avoid aggravating your back. By session 4 or 5, you’re doing more active exercises. Most people report feeling 80-90% better by session 6.
Chronic pain is a longer road. You’ll likely need 15 to 25 sessions over 8 to 12 weeks. The first few sessions are about learning. You’ll talk. You’ll ask questions. You’ll get handouts. You’ll learn why your pain persists even though your back looks fine on an MRI. Then comes the movement work-slow, controlled, and designed to rebuild your confidence. Progress isn’t linear. Some weeks feel better. Others feel like backsliding. That’s normal. The goal isn’t to feel zero pain. It’s to feel in control.
Success isn’t measured by pain scores alone. It’s measured by what you can do: walk the dog, play with your kids, sit through a movie, go back to work. If you can do those things-even with some discomfort-you’ve won.

The Bigger Picture: Why This Matters
Low back pain is the #1 cause of disability worldwide. In the U.S. alone, it costs over $100 billion a year. But here’s the hopeful part: most of it is preventable. And physical therapy is the most cost-effective, evidence-backed tool we have.
Medicare and insurers are finally catching on. New reimbursement rules now reward physical therapists who help patients avoid chronic pain. Digital tools like Kaia Health, an FDA-cleared app that guides you through PT exercises at home, are becoming mainstream. And tools like the Back Pain Stratification Tool can now predict-with 83% accuracy-who’s at risk of turning acute pain into chronic pain. That means earlier, smarter intervention.
This isn’t just about individual recovery. It’s about changing a broken system that too often waits until pain becomes permanent before acting. The future of back pain care isn’t pills or surgery. It’s education, movement, and timing.
What You Can Do Right Now
- If your back pain started in the last week: Call a physical therapist today. Don’t wait. Don’t rest for days. Start moving-safely.
- If you’ve had pain for more than 3 months: Look for a therapist trained in pain neuroscience. Ask if they use the STarT Back approach or offer pain education. If they don’t, keep looking.
- If you’re scared to move: That’s normal. But it’s also the biggest barrier to recovery. Your therapist isn’t there to make you hurt. They’re there to prove you’re safe.
- If you’ve been told your pain is "all in your head": It’s not. Your pain is real. But your nervous system is misfiring. That’s fixable.
Low back pain doesn’t have to be a life sentence. Whether it’s new or lingering, the right approach makes all the difference. The clock is ticking. Start moving-before your body forgets how.
How do I know if my back pain is acute or chronic?
Acute low back pain lasts less than 4 weeks and usually follows a clear injury-like lifting something heavy or twisting awkwardly. It’s sharp, localized, and often improves with rest and movement. Chronic pain lasts longer than 12 weeks (or 6 months, depending on the guideline). It’s often dull, persistent, and may not have a clear cause. If your pain is still here after 3 months, it’s likely chronic. The key difference isn’t just time-it’s how your nervous system is responding.
Can physical therapy really prevent acute back pain from becoming chronic?
Yes, and the evidence is strong. Starting physical therapy within 14 days of acute pain onset reduces the chance of chronic pain by 16-22%. When treatment begins within 72 hours, chronicity risk drops by 22%. Early PT teaches your body to move safely, prevents muscle guarding, and stops your nervous system from becoming hypersensitive. Waiting too long increases the risk by 38%.
Why doesn’t physical therapy always work for chronic back pain?
It’s not that PT doesn’t work-it’s that many therapists still treat chronic pain like acute pain. If you’re only doing stretches and strengthening without addressing fear, stress, and nervous system sensitivity, you’re missing the core issue. Chronic pain often involves central sensitization, where the brain amplifies pain signals. The most effective therapy includes pain neuroscience education, graded exposure, and cognitive strategies. Look for therapists with training in these areas.
Should I get an MRI if I have chronic back pain?
Usually, no. Most people with chronic back pain have changes on MRI-like disc degeneration or bulges-that are also found in people with zero pain. These findings don’t explain the pain. Getting an MRI too early can lead to unnecessary worry, more tests, and even unnecessary surgery. Physical therapy should be the first step. Imaging is only helpful if there are red flags: loss of bladder control, leg weakness, or unexplained weight loss.
Is it safe to move when my back hurts?
Yes-especially if it’s acute. Resting for more than 2-3 days actually delays recovery. Gentle movement improves blood flow, reduces stiffness, and tells your brain you’re safe. For chronic pain, movement might feel scary, but avoiding it makes your nervous system more sensitive. A good physical therapist will guide you through safe, graded movements that slowly rebuild your confidence. Pain during movement doesn’t mean damage-it often means sensitivity. That’s something you can retrain.
What should I look for in a physical therapist for back pain?
For acute pain, look for someone skilled in mechanical diagnosis (like MDT or McKenzie method). For chronic pain, find someone trained in pain neuroscience education, cognitive functional therapy, or the STarT Back approach. Ask if they explain why pain persists beyond tissue healing. Avoid therapists who rely on passive treatments (like ultrasound or massage) without a plan. The best ones teach you how to manage your pain, not just relieve it.
Next Steps: What to Do If You’re Stuck
If you’re still in pain after physical therapy, ask yourself: Did I get the right kind of therapy? Was it early enough? Did my therapist explain the science behind my pain? If the answer is no, it’s not you-it’s the approach.
Consider seeking out a specialist in chronic pain rehabilitation. These clinics often include psychologists, occupational therapists, and pain educators working together. They don’t just fix your back-they help you rebuild your life around it.
And if you’re feeling discouraged? You’re not alone. But you’re not broken. Chronic pain is a complex condition-not a personal failure. The tools to manage it exist. You just need the right guide.


pragya mishra
Stop wasting time with PT if you're not willing to move. I had chronic pain for 5 years, did every stretch, every massage, every 'neuroscience lecture' - still hurt. Then I lifted weights. Heavy. Daily. Pain vanished. Your nervous system doesn't need education - it needs to be proven wrong by force.