Medication-Induced Psychosis Risk Checker
Quick Risk Assessment
Answer these questions to determine your risk of medication-induced psychosis.
What Is Medication-Induced Psychosis?
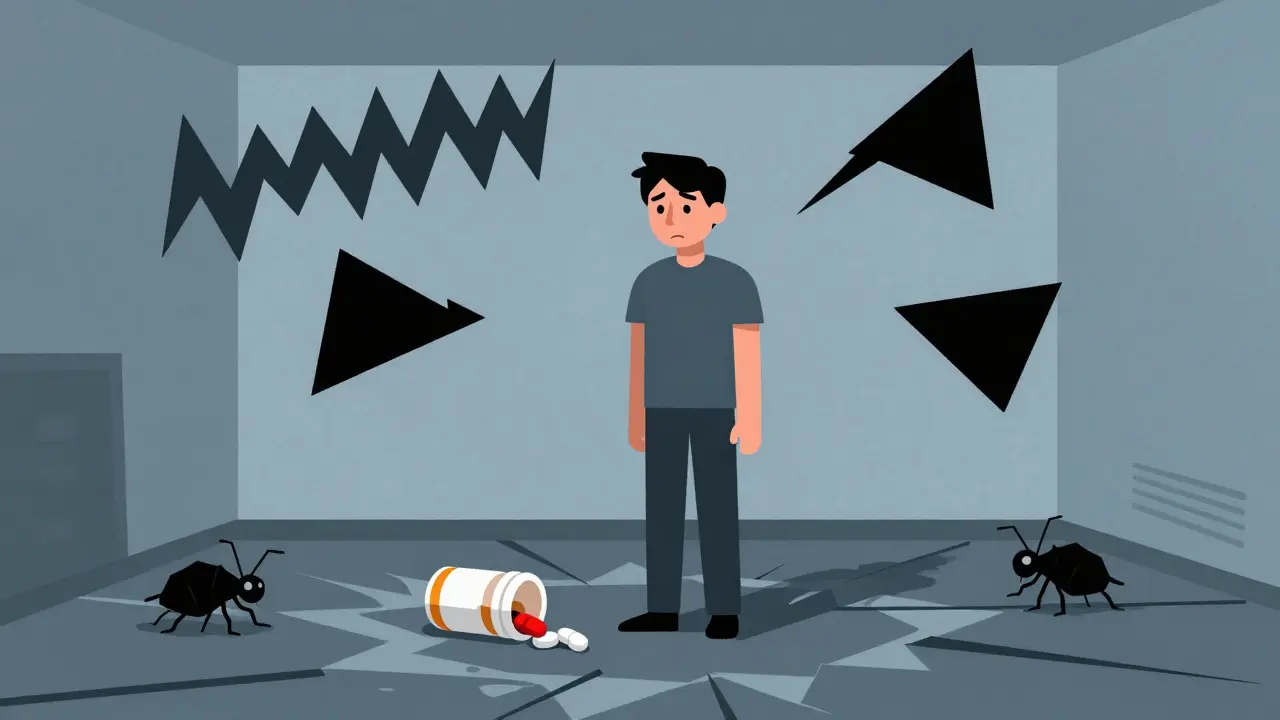
Medication-induced psychosis isn’t something you grow into-it happens fast. One day you’re taking a pill for your back pain, your depression, or even malaria prevention, and the next, you’re hearing voices, convinced someone’s watching you, or seeing things that aren’t there. This isn’t schizophrenia. It’s not a lifelong mental illness. It’s your body reacting to a drug, and it can happen to anyone-even people with no history of mental health issues.
The DSM-5, the standard guide doctors use to diagnose mental conditions, defines it clearly: psychotic symptoms must appear during or within a month of taking a medication, or during withdrawal. That’s the key. If the hallucinations or delusions stick around longer than a month after stopping the drug, then something else might be going on. But if they fade? That’s medication-induced psychosis.
What Does It Actually Look Like?
The symptoms are terrifying because they feel real. You’re not imagining that you’re in danger-you truly believe it. Common signs include:
- Delusions: Strong false beliefs, especially paranoia (like thinking neighbors are spying on you or that your phone is being hacked)
- Hallucinations: Hearing voices (most common), seeing shadows move, feeling bugs crawling on your skin
- Disorganized speech: Jumping from topic to topic, saying things that don’t connect
- Confusion: Forgetting where you are, not recognizing loved ones
- Agitation or aggression: Sudden outbursts, pacing, or violent behavior
- Emotional flatness or extreme anxiety: Some people become numb; others are in panic mode
These don’t always show up at once. Often, mood changes come first-intense irritability, panic attacks, or deep depression-before full psychosis kicks in. That’s your warning sign. If you or someone you know starts acting strangely after starting a new medication, don’t wait.
Which Medications Can Trigger This?
It’s not just street drugs. Prescription meds are the biggest culprit. Here are the most common offenders:
- Corticosteroids (like prednisone): Used for asthma, arthritis, autoimmune diseases. About 1 in 20 people on high doses develop psychosis. It’s not rare-it’s underreported.
- Antimalarials (like mefloquine): Travelers taking this for malaria prevention have reported vivid nightmares, paranoia, and hallucinations. The European Medicines Agency has logged over 1,200 cases since the 1980s.
- Antiretrovirals (like efavirenz): Used for HIV. About 1 in 40 patients experience severe psychiatric side effects, including psychosis.
- Antidepressants (SSRIs/SNRIs): Rare, but possible. Especially in younger people or those with bipolar disorder undiagnosed.
- Stimulants (methylphenidate, amphetamines): Used for ADHD. High doses can cause paranoia and hallucinations that mimic cocaine psychosis.
- Antiepileptics (like vigabatrin): Can cause psychosis in over 1% of users.
- Antihistamines (like diphenhydramine): Found in sleep aids and cold meds. High doses or interactions can trigger confusion and hallucinations.
- Opioids and NSAIDs: Even ibuprofen in very high doses has been linked to psychotic episodes.
And yes-cannabis. About 1 in 10 regular users will experience psychotic symptoms. If you’ve never had mental health issues before, but you start using cannabis heavily, your risk goes up.
Who’s Most at Risk?
It’s not random. Certain people are more vulnerable:
- Those with a personal or family history of schizophrenia or bipolar disorder
- Women: Studies show higher rates of medication-induced psychosis in women, especially with steroids and antimalarials
- People with substance use disorders: 74% of those hospitalized for first-time psychosis had a history of drug or alcohol abuse
- Older adults: More likely to be on multiple meds, and their bodies process drugs slower
- People taking multiple drugs at once: Interactions can turn a safe dose into a dangerous one
Even if you’ve taken a drug before without issue, that doesn’t mean it won’t trigger psychosis this time. Your body changes. Your liver slows down. Your stress levels rise. The trigger can show up out of nowhere.

Emergency Response: What to Do Right Now
If someone is experiencing acute psychosis from medication, time matters. Don’t wait. Don’t try to reason with them. Don’t argue about whether the voices are real. Their brain is in crisis.
- Call emergency services immediately if there’s any risk of harm-to themselves or others. Say clearly: “They’re having a drug-induced psychotic episode.”
- Remove the medication if you can do it safely. Don’t let them take another dose.
- Stay calm and present. Speak in a quiet, steady voice. Say: “I’m here. You’re safe. We’re getting help.”
- Do not restrain unless absolutely necessary. Physical struggle can trigger more fear and aggression.
- Bring the medication bottles to the hospital. This is critical. Doctors need to know exactly what was taken, when, and how much.
Hospitals will check for other causes-brain infections, metabolic imbalances, withdrawal from alcohol or benzodiazepines. But if it’s medication-induced, the first step is always stopping the drug.
How Is It Treated in the ER?
There’s no magic pill, but there are proven steps:
- Stop the drug: This is the single most effective treatment. For many, symptoms fade within hours to days.
- Supportive care: IV fluids, electrolytes, monitoring heart rate and temperature. Stimulant-induced psychosis can cause dangerous overheating or muscle breakdown.
- Antipsychotics: Olanzapine or quetiapine are often given in low doses to calm hallucinations and delusions. But doctors are careful-they don’t want to mask symptoms or cause bad interactions.
- For withdrawal psychosis (alcohol, benzos): Benzodiazepines like lorazepam are used to prevent delirium tremens, which can be deadly.
Important: Antipsychotics aren’t always needed. If symptoms are mild and the drug is stopped, they often resolve without medication. Overmedicating can delay recovery and create new problems.
Recovery and What Comes Next
Most people recover fully-if they stop the drug early.
- Steroid psychosis: Usually clears in 4 to 6 weeks
- Cocaine or methamphetamine psychosis: Often gone in 24 to 72 hours
- Alcohol-related psychosis: Can take weeks, especially if there’s brain damage from long-term use
But here’s the catch: 7 to 10% of people who show up in ERs with first-time psychosis are later found to have an underlying disorder like schizophrenia. That’s why follow-up is non-negotiable.
Doctors recommend psychiatric check-ins for at least 3 months after symptoms disappear. If the psychosis returns after stopping the drug, it’s a red flag. You need a full mental health evaluation.
How to Prevent It
Prevention starts with awareness:
- Ask your doctor: “Can this medication cause psychosis?” before starting any new drug.
- Know your family history. If someone in your family has schizophrenia or bipolar disorder, be extra cautious with stimulants, steroids, or antidepressants.
- Keep a medication log: Write down every pill you take, including OTC drugs and supplements. Bring it to every appointment.
- Don’t mix meds without checking. Even something as simple as cold medicine with antidepressants can be risky.
- Watch for early signs: Mood swings, sleep problems, anxiety spikes-these can be the first warning.
- Read the patient information leaflets. The FDA requires warnings for drugs like efavirenz and mefloquine. If it says “contact your doctor if you feel depressed or paranoid,” take it seriously.
When to Worry: A Quick Checklist
If you or someone you care about is on medication and shows any of these, seek help immediately:
- Starts hearing voices or seeing things others don’t
- Becomes convinced someone is trying to hurt them
- Stops sleeping, eating, or caring for themselves
- Starts acting aggressively or erratically
- Has a recent change in medication-within the last 30 days
Can over-the-counter meds cause psychosis?
Yes. First-generation antihistamines like diphenhydramine (found in Benadryl, sleep aids, and cold meds) can cause hallucinations and confusion, especially in older adults or when taken in high doses. Decongestants like pseudoephedrine can also trigger anxiety and paranoia in sensitive individuals. Always check the label for psychiatric side effects.
Is medication-induced psychosis permanent?
In most cases, no. Symptoms usually resolve within days to weeks after stopping the drug. But if the person had a hidden mental illness, like schizophrenia, the psychosis may return even after the medication is gone. That’s why follow-up care is essential-doctors need to rule out underlying conditions.
Can you get psychosis from stopping a medication?
Absolutely. Withdrawal from alcohol, benzodiazepines, and even some antidepressants can trigger psychosis. This is why you should never stop these drugs cold turkey. Always taper under medical supervision. Withdrawal psychosis can be mistaken for a relapse of schizophrenia, but it’s often temporary if managed correctly.
Why do doctors sometimes miss this diagnosis?
Because psychosis is usually assumed to be psychiatric, not medical. Many doctors don’t ask about recent medication changes, especially if the patient is on common drugs like steroids or antidepressants. A 2019 study found only 38% of primary care doctors felt confident diagnosing drug-induced psychosis. That’s why patients and families need to speak up: “I started this drug two weeks ago, and now I’m hearing voices.” That detail saves lives.
Does this mean I can never take that medication again?
If you’ve had psychosis from a specific drug, you should avoid it in the future. Re-exposure can trigger it again-sometimes more severely. But it doesn’t mean you can’t take similar drugs. For example, if prednisone caused psychosis, another steroid might be safe at a lower dose. Talk to a specialist. Genetic testing for drug metabolism is becoming more available and may help predict risk in the future.
Final Thought: Trust Your Instincts
If something feels off after starting a new medication, it probably is. Psychosis doesn’t always come with a warning label. It sneaks in-sometimes after one dose, sometimes after months. But it’s treatable. And it’s often reversible. The key is catching it early. Don’t wait for someone to “snap out of it.” Don’t assume it’s just stress. Call a doctor. Call 911. Your quick action could be the difference between a full recovery and a lifelong diagnosis.

Ted Conerly
Just had a friend go through this after a steroid course for a bad flare-up. One week she was fine, next week she was convinced the neighbors were bugging the house. Took her three days to calm down after stopping the meds. This post is spot on. If you see sudden paranoia or hallucinations after a new prescription, don’t wait. Call the doctor immediately.