Steroid Dose Bone Loss Calculator
Your Steroid Risk Assessment
Why Your Bones Are at Risk on Long-Term Steroids
If you’ve been on prednisone or another corticosteroid for more than three months, your bones are likely losing density-fast. This isn’t just a side effect you have to live with. It’s glucocorticoid-induced osteoporosis (GIOP), the most common form of secondary osteoporosis, and it can turn a routine prescription into a fracture waiting to happen. Within just three to six months of starting steroids, your fracture risk jumps by 70% to 100%. Bone mineral density can drop by 5% to 15% in the first year, especially in your spine. And unlike age-related bone loss, this happens quickly, silently, and often without warning.
The problem isn’t just that steroids weaken bones. They attack the system from multiple angles. They reduce how much calcium your body absorbs from food by about 30%. They make your kidneys dump more calcium instead of holding onto it. They shut down the cells that build new bone (osteoblasts) and keep the cells that break bone down (osteoclasts) alive longer. Even worse, they make your bones less responsive to weight-bearing exercise-meaning walking or lifting weights gives you less benefit than it used to.
Who’s Really at Risk? It’s Not Just the Elderly
You don’t have to be older to be in danger. The moment you hit a daily prednisone dose of 2.5 mg or more for three months or longer, you enter the high-risk zone. That’s the threshold set by the Royal Osteoporosis Society and the American College of Rheumatology. And if you’re taking 7.5 mg or more per day? Your fracture risk doubles. For every extra milligram of prednisone you take each day, you lose another 1.4% of bone density in your spine annually. That’s not a slow decline-it’s a steady erosion.
And here’s the kicker: men are far less likely to get screened or treated than women. One study found only 44% of men on long-term steroids received any kind of bone health intervention, compared to 76% of women. That gap isn’t because men are less at risk-it’s because doctors assume osteoporosis is a ‘woman’s issue.’ It’s not. Men on steroids lose bone just as fast, and they’re more likely to die from a hip fracture.
Step 1: Lower the Dose-If You Can
The single most effective thing you can do? Reduce your steroid dose to the lowest level that still controls your condition. Cutting your daily prednisone from over 7.5 mg down to 7.5 mg or less can cut your fracture risk by 35% in just six months. That’s not a small win. That’s life-changing.
But you can’t just stop steroids cold. If you have rheumatoid arthritis, lupus, or another autoimmune disease, your doctor will work with you to taper slowly. Sometimes, switching to a different medication or using steroid-sparing drugs like methotrexate or biologics can help. Don’t assume you’re stuck with high doses forever. Ask your doctor: Is there a way to reduce this dose without risking a flare?
Step 2: Calcium and Vitamin D-Non-Negotiable
Supplements aren’t optional here. They’re the bare minimum. The Cleveland Clinic and the American College of Rheumatology agree: everyone on long-term steroids needs 1,000 to 1,200 mg of calcium and 600 to 800 IU of vitamin D daily. Some people need up to 1,000 IU of vitamin D to keep their blood levels above 20 ng/mL-the minimum for bone protection.
Try to get calcium from food first: dairy, leafy greens, fortified plant milks, canned salmon with bones. But most people won’t hit the target without supplements. Vitamin D is trickier. Even in sunny Melbourne, many people on steroids are deficient because steroids interfere with how your body uses it. A simple blood test can check your levels. If you’re below 30 ng/mL, your doctor should bump up your dose.
Studies show that taking 1,000 mg calcium and 500 IU vitamin D together prevents 0.72% annual bone loss in the spine. Without it, you lose about 2% per year. That’s the difference between staying stable and heading toward a fracture.
Step 3: Move Your Body-Even If It Feels Hard
Exercise isn’t just ‘good for you’-it’s medical treatment. Weight-bearing activity like walking, stair climbing, or resistance training tells your bones to stay strong. But steroids blunt that signal. You still need to move, but you might need to work harder to get the same effect.
Shoot for at least 30 minutes of weight-bearing exercise on most days. If your joints hurt, try swimming or cycling for cardio, but add in light weights or resistance bands two to three times a week. Don’t skip strength training-it’s your best defense against spine and hip fractures. And if you’re unsure where to start, ask your doctor for a referral to a physiotherapist who understands steroid-related bone loss.
Step 4: Medications That Actually Work
If you’re at moderate to high risk-based on your dose, age, previous fractures, or bone density test-you need more than calcium and exercise. You need a prescription.
Bisphosphonates like risedronate (5 mg daily or 35 mg weekly) are the first-line treatment. They cut vertebral fracture risk by 70% and non-vertebral fractures by 41%. Zoledronic acid, given as an annual IV drip, boosts spine bone density by 4.5% in just 12 months. Denosumab, a twice-yearly injection, increases spine density by 7%. And if you’ve already had a fracture or have a T-score below -2.5, teriparatide (a daily injection) is the strongest option-it increases spine density by 9.1% in a year, more than double what bisphosphonates achieve.
Teriparatide isn’t for everyone. It’s expensive and usually limited to two years of use. But for people with severe bone loss, it’s often the only thing that rebuilds bone fast enough to prevent another fracture.

Why Most People Don’t Get Help-And How to Fix It
Here’s the uncomfortable truth: only about 15% of people on long-term steroids get care that matches the guidelines. Why? Because doctors don’t always know what to do. Only 22% of primary care providers feel confident managing steroid-induced bone loss. Patients think it’s inevitable. One study found 45% believe bone loss from steroids is unavoidable.
And the numbers don’t lie: only 31% of patients get a bone density scan. Only 40% are documented as taking calcium. Only 37% are on vitamin D. That’s not negligence-it’s a system failure.
But change is possible. One hospital system in the U.S. Veterans Affairs network used automated alerts in electronic records. When a patient got a steroid prescription over 2.5 mg/day for three months, the system flagged it and pushed a checklist: check BMD, prescribe calcium/vitamin D, assess fracture risk. Result? Intervention rates jumped from 40% to 92%. That’s proof that with the right systems, you can fix this.
What You Need to Do Right Now
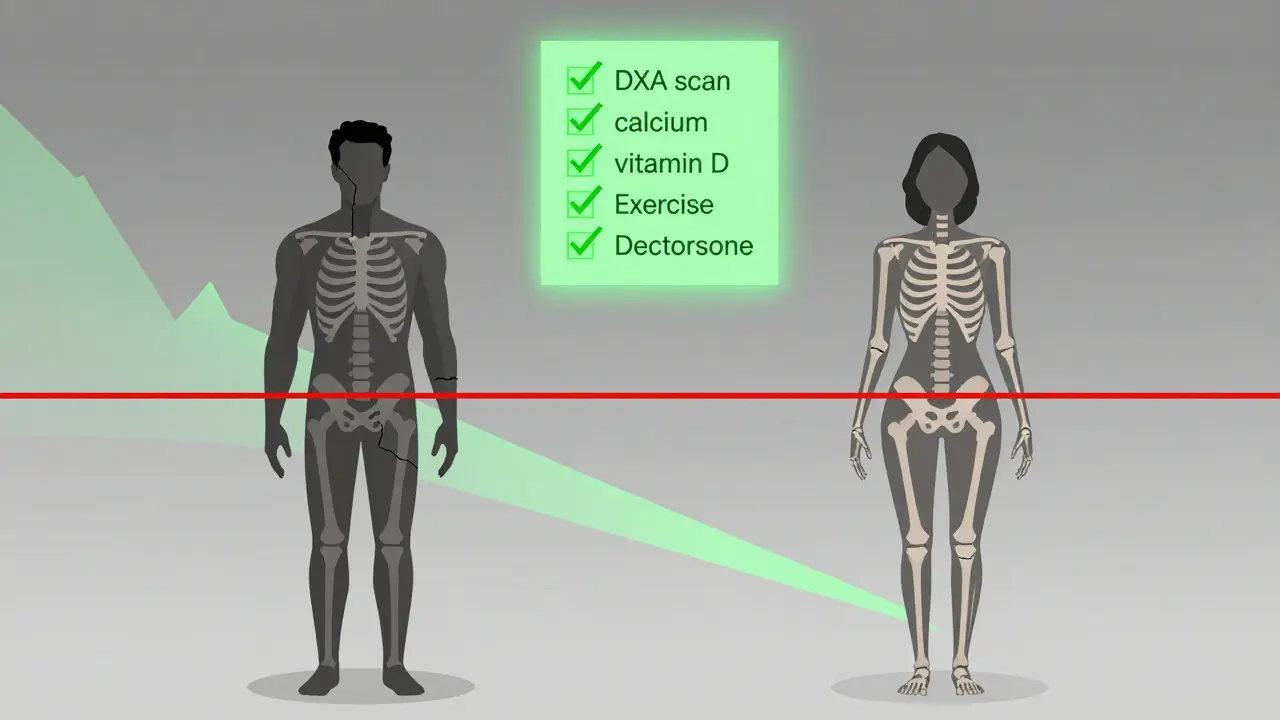
If you’re on steroids for three months or longer, here’s your action list:
- Ask your doctor for a bone density scan (DXA) now, and again every one to two years.
- Get your vitamin D level checked. If it’s under 30 ng/mL, ask for a higher dose.
- Take 1,000-1,200 mg calcium and 800 IU vitamin D daily-no exceptions.
- Start or maintain weight-bearing exercise. If you’re not doing it, start today.
- Ask: ‘Can my steroid dose be lowered?’ and ‘Do I need a bone medication?’
- If you’ve had a fracture, or your T-score is below -2.5, ask about teriparatide.
Don’t wait for a broken bone to act. Half of all steroid-related fractures happen in the first year. Prevention isn’t about being careful-it’s about being proactive.
Adherence Is the Biggest Hurdle-Here’s How to Beat It
Even when you know what to do, sticking to it is hard. Pharmacy records show only 40% of patients are still taking calcium and vitamin D after a year. Bisphosphonate adherence drops from 65% at six months to 45% at one year. Why? Stomach upset. The pills can irritate your esophagus. That’s why many people stop.
Here’s what works: switch to the weekly pill instead of daily. Or ask about the IV version-zoledronic acid once a year. No swallowing pills. No stomach issues. Or try denosumab injections every six months. If GI side effects are your problem, talk to your doctor about alternatives. Don’t give up because the first option didn’t work.
Also, get support. A pharmacist-led education program in one clinic boosted guideline adherence from 35% to 85% in six months. You don’t have to figure this out alone.


Tony Du bled
I've been on prednisone for 2 years. Bone scan showed -2.8. Started calcium + D3, walked daily, and got the yearly zoledronic acid. No fractures. Simple as that.