Why Renal Ultrasound Is the First Step When Kidneys Don’t Look Right
If your doctor suspects a blockage in your urinary tract or thinks your kidneys might be swollen, shrinking, or under pressure, they’ll almost always start with a renal ultrasound. It’s quick, safe, and doesn’t use radiation. Unlike CT scans or MRIs, you don’t need to fast, drink contrast dye, or lie in a tight tube. You just lie on your back or side while a technician moves a small device over your flank - and in 15 to 30 minutes, they get a clear picture of your kidneys’ size, shape, and whether urine is backing up.
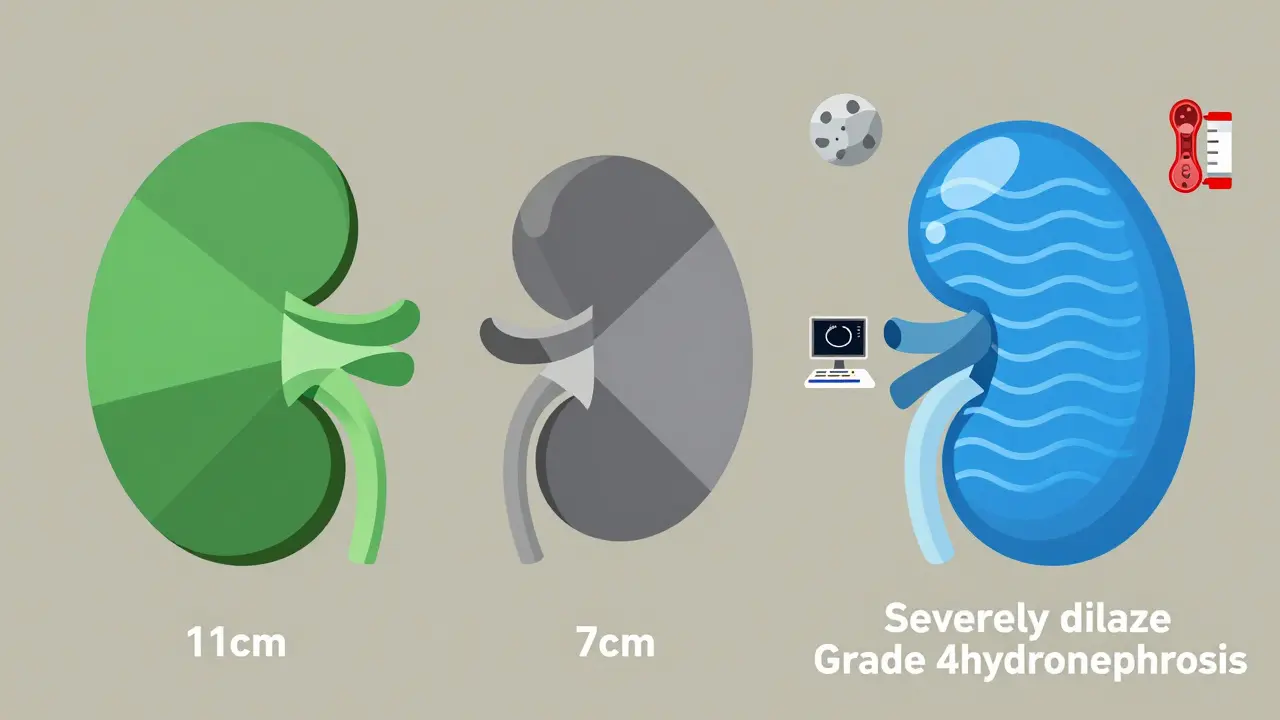
This isn’t just a basic check-up. Renal ultrasound gives real, measurable data. Is your right kidney 11 cm long? Is the cortex thicker than 1 cm? Is the renal pelvis dilated beyond 7 mm? These numbers matter. They tell doctors whether you’re dealing with a mild, temporary issue - like a small stone passing - or something more serious, like a long-term blockage at the ureteropelvic junction (UPJ) that could damage your kidney over time.
What Exactly Does a Renal Ultrasound Show?
A renal ultrasound doesn’t just show a blurry outline of your kidneys. It gives precise measurements and reveals hidden problems. Here’s what it looks for:
- Kidney length: Normal adult kidneys are 9 to 13 cm long. A kidney smaller than 8 cm might mean chronic damage, while one larger than 14 cm could signal swelling from obstruction or a tumor.
- Cortical thickness: The outer layer of the kidney (cortex) should be at least 1 cm thick. If it’s thinner, your kidney may have lost functional tissue - often from long-standing high blood pressure, diabetes, or untreated obstruction.
- Renal pelvis diameter: The central collecting area of the kidney should be less than 7 mm wide. If it’s wider, that’s hydronephrosis - urine is pooling because it can’t drain properly.
- Hydronephrosis grade: Doctors use the Society for Fetal Urology scale (grades 0 to 4) to describe how bad the swelling is. Grade 1 is mild, just a little dilation. Grade 4 means the kidney looks like a balloon filled with fluid - a red flag for urgent intervention.
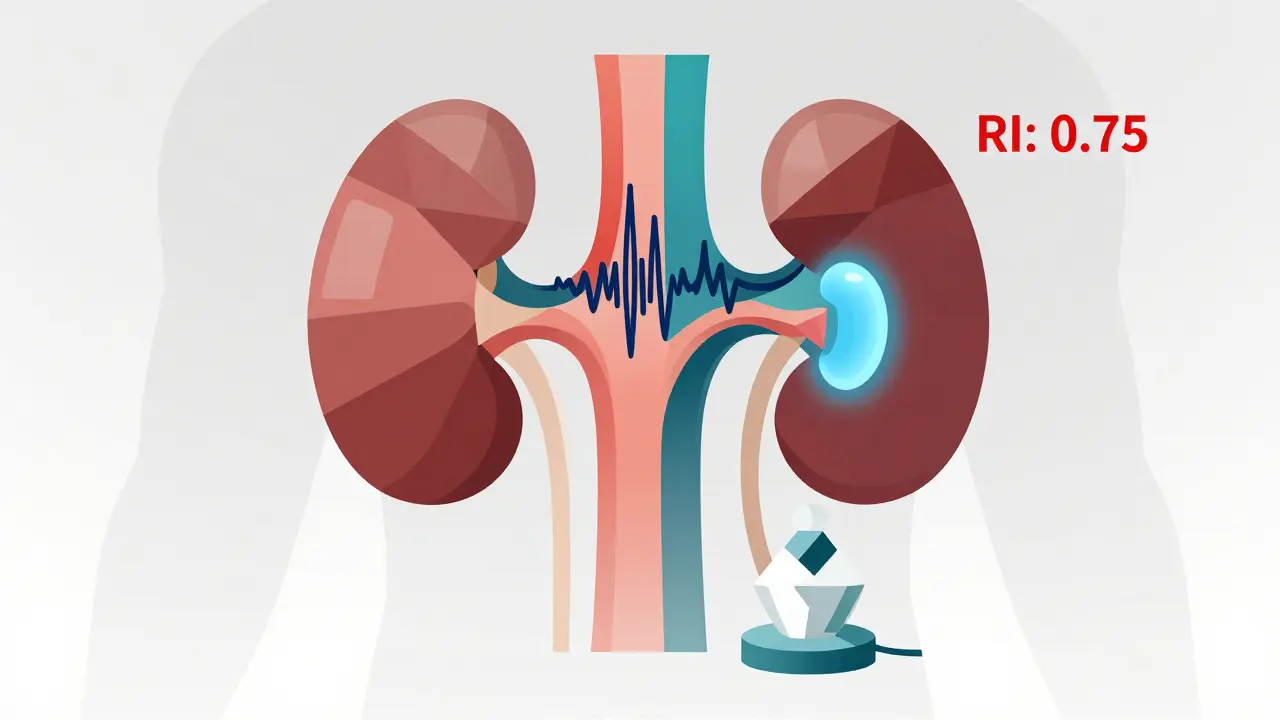
- Resistive index (RI): This is where ultrasound gets powerful. Using Doppler, it measures blood flow resistance in the kidney’s arteries. A normal RI is below 0.70. If it’s 0.70 or higher, it strongly suggests obstruction is putting pressure on the kidney’s blood supply. Studies show this test is 86.7% sensitive and 90% specific for detecting blockages.
These aren’t just guesses. They’re numbers backed by years of clinical research. A 2015 study in the Nigerian Journal of Clinical Practice confirmed that an RI above 0.70 is a reliable marker for obstructive uropathy - even before the kidney starts to look visibly enlarged.
How It Compares to CT Scans and MRIs
CT scans are great for finding tiny kidney stones - down to 1-2 mm. But they expose you to about 10 millisieverts of radiation. That’s like getting 500 chest X-rays. For someone with recurrent stones or a child with suspected UPJ obstruction, repeated CT scans add up fast. MRIs give detailed soft-tissue images but cost 3 to 5 times more than ultrasound and still can’t reliably detect small stones.
Renal ultrasound doesn’t replace CT or MRI - it leads the way. Here’s the practical difference:
| Feature | Renal Ultrasound | CT Urography | Magnetic Resonance Urography (MRU) |
|---|---|---|---|
| Detects small stones (<3 mm) | No (misses ~20%) | Yes | No |
| Measures kidney size and hydronephrosis | Yes, accurately | Yes | Yes |
| Measures blood flow (Doppler/RI) | Yes | No | Yes, but rarely used |
| Radiation exposure | None | High (~10 mSv) | None |
| Cost (USD, 2023) | $200-$500 | $800-$1,500 | $1,500-$2,500 |
| Best for | First-line, pregnant patients, kids, monitoring | Emergency stone detection, complex anatomy | Patients who can’t have radiation or contrast |
Emergency rooms use point-of-care ultrasound to cut diagnosis time by 45 minutes. A patient with severe flank pain gets scanned at the bedside. If hydronephrosis is seen, they’re fast-tracked for treatment. No waiting for a radiology slot. No radiation risk. Just fast, safe action.
When Ultrasound Falls Short
Ultrasound isn’t perfect. It’s highly dependent on the operator’s skill and the patient’s body type. If you have a BMI over 35, the sound waves can’t penetrate deeply enough to get a clear image. In those cases, doctors have to switch to CT or MRI - even if it means more radiation or higher cost.
Another issue? Bowel gas. If your intestines are full of air, they can block the ultrasound beam and hide parts of the kidney. That’s why technicians often ask you to drink water before the scan - a full bladder pushes the bowel out of the way and gives a clearer view.
And then there’s the learning curve. A 2018 study found that inexperienced sonographers could mismeasure kidney length by up to 20%. That’s a big deal if you’re tracking kidney shrinkage over time. The American College of Radiology recommends at least 50 supervised exams before a tech can reliably measure resistive index. That’s why many hospitals now use AI-assisted tools to help standardize measurements - especially for hydronephrosis grading.
What Happens After the Scan?
Once the ultrasound is done, the results are interpreted in context. A single enlarged kidney with high RI? That’s a red flag for acute obstruction - maybe a stone stuck in the ureter. If both kidneys are swollen, it could point to a blockage lower down, like in the bladder or urethra.
For patients with known UPJ obstruction, ultrasound is used weekly or monthly to track progress. One urologist in Melbourne told me: “I’d rather use ultrasound to watch a child’s kidney over six months than expose them to five CT scans.” That’s the real power of this tool - it’s safe enough to use again and again.
If the ultrasound shows mild hydronephrosis with normal RI, the doctor might just wait and recheck in a few weeks. If RI is high or the kidney is shrinking, they’ll order a CT or MRU to plan surgery. In some cases, they’ll even use advanced techniques like shear-wave elastography - which measures how stiff the kidney tissue has become due to pressure - to predict if the damage is reversible.
The Future: AI, Super-Resolution, and Quantitative Ultrasound
Renal ultrasound isn’t standing still. New research is turning it into a quantitative tool, not just a visual one.
Super-resolution ultrasound imaging, described in a 2024 Nature Reviews Nephrology article, is now being tested to count tiny blood vessels in the kidney. This could detect early signs of fibrosis - scarring - before kidney function drops. That’s huge. Right now, we only know a kidney is failing when creatinine rises. Soon, we might see the damage before it happens.
AI is also stepping in. Mayo Clinic is running trials where software automatically grades hydronephrosis. No human interpretation needed. Just upload the scan, and the algorithm gives a grade. Early results are promising - accuracy matches expert radiologists.
And then there’s ultrasound localization microscopy (ULM). It’s still experimental, but it could one day let doctors count individual nephrons - the filtering units of the kidney - without a biopsy. Imagine knowing exactly how many functional units you have left. That’s the future.

Who Needs This Test Most?
Renal ultrasound isn’t for everyone. But it’s essential for:
- Patients with sudden, severe flank pain - especially if they have a history of kidney stones.
- Pregnant women with urinary symptoms - radiation is avoided at all costs.
- Children with suspected UPJ obstruction - repeated imaging is common, so safety matters.
- People with chronic kidney disease - tracking kidney size over time shows progression.
- Post-surgery patients - like those who had a pyeloplasty for UPJ obstruction - to make sure the repair holds.
If you’re over 50, have high blood pressure, or diabetes, and your doctor notices your creatinine is rising, they might order an ultrasound to see if your kidneys are shrinking - a sign of long-term damage.
What to Expect During the Exam
You won’t feel much. You’ll lie on your back or side. A gel is applied to your flank. The technician moves the probe slowly, taking pictures from different angles. You might be asked to hold your breath briefly or change position. It’s painless. No needles. No radiation. No waiting.
Drink water before the scan if instructed - a full bladder helps push the bowel away and gives a clearer view of the kidneys and ureters. You don’t need to fast. You can eat normally. Just wear loose clothing.
The whole thing takes 15 to 30 minutes. Results are usually available within a day. Your doctor will compare the measurements to normal ranges and look at trends - especially if you’ve had ultrasounds before.
Final Thought: It’s Not Just a Picture - It’s a Measurement Tool
Renal ultrasound isn’t just about seeing your kidneys. It’s about measuring them. Tracking them. Understanding how pressure changes blood flow. Knowing when a kidney is under stress - even before it hurts.
It’s the safest, most repeatable, most cost-effective way to start investigating kidney problems. And with AI and new imaging techniques on the rise, it’s only getting smarter. For now, it remains the undisputed first step - not because it’s perfect, but because it’s the best place to begin.
Can renal ultrasound detect kidney stones?
Yes, but not always. Ultrasound detects about 80% of kidney stones larger than 3 mm. It’s less reliable for tiny stones under 2 mm - that’s where CT scans are better. However, ultrasound is still the first test because it shows if a stone is causing a blockage (hydronephrosis), even if the stone itself isn’t visible.
Is renal ultrasound safe during pregnancy?
Yes, it’s the safest imaging option during pregnancy. Unlike CT or X-rays, it uses sound waves, not radiation. It’s routinely used to check for kidney obstruction, hydronephrosis, or infection in pregnant women with flank pain.
What does a high resistive index mean?
A resistive index (RI) of 0.70 or higher suggests increased resistance to blood flow in the kidney, often caused by obstruction. It’s a strong indicator that urine is backing up and putting pressure on the kidney’s blood vessels. An RI above 0.70 has been shown to be 86.7% sensitive and 90% specific for obstructive uropathy.
Can obesity affect the results of a renal ultrasound?
Yes. In patients with a BMI over 35, ultrasound waves can’t penetrate deeply enough to get clear images of the kidneys. In these cases, doctors often need to use CT or MRI instead, even though those involve radiation or higher cost.
How often can you have a renal ultrasound?
As often as needed. Because it uses no radiation, it’s safe for repeated use. Patients with chronic obstruction, like those with UPJ syndrome or post-surgery follow-up, often have ultrasounds every few weeks or months to track kidney size and hydronephrosis without risk.
Do I need to prepare for a renal ultrasound?
Usually, you’ll be asked to drink water 30-60 minutes before the scan to fill your bladder. This helps push bowel gas out of the way and gives a clearer view of the kidneys and ureters. You don’t need to fast. Wear loose clothing that allows access to your sides.

Shelby Price
I had a renal ultrasound last year after a kidney stone scare. Honestly, it was way less scary than I thought. No needles, no weird drinks, just some gel and a little pressure. The tech even let me see the image on the screen - my kidney looked like a little bean with a tiny balloon inside. Weirdly comforting?