Topical steroids are one of the most common treatments for eczema, psoriasis, and other inflamed skin conditions. They work fast, often clearing redness and itching in just a few days. But if you use them the wrong way - too long, too often, or on the wrong part of your body - you risk skin thinning, a real and sometimes permanent side effect. The good news? Most people never experience it when they follow simple, evidence-based rules. The problem isn’t the medication. It’s how it’s used.
What Topical Steroids Actually Do
Topical corticosteroids are anti-inflammatory drugs applied directly to the skin. They don’t cure eczema or psoriasis, but they silence the immune response causing flare-ups. Unlike oral steroids, which flood your whole body, topical versions mostly stay on the skin. Your skin cells break down most of the steroid before it enters your bloodstream. That’s why they’re safer than pills for localized problems.
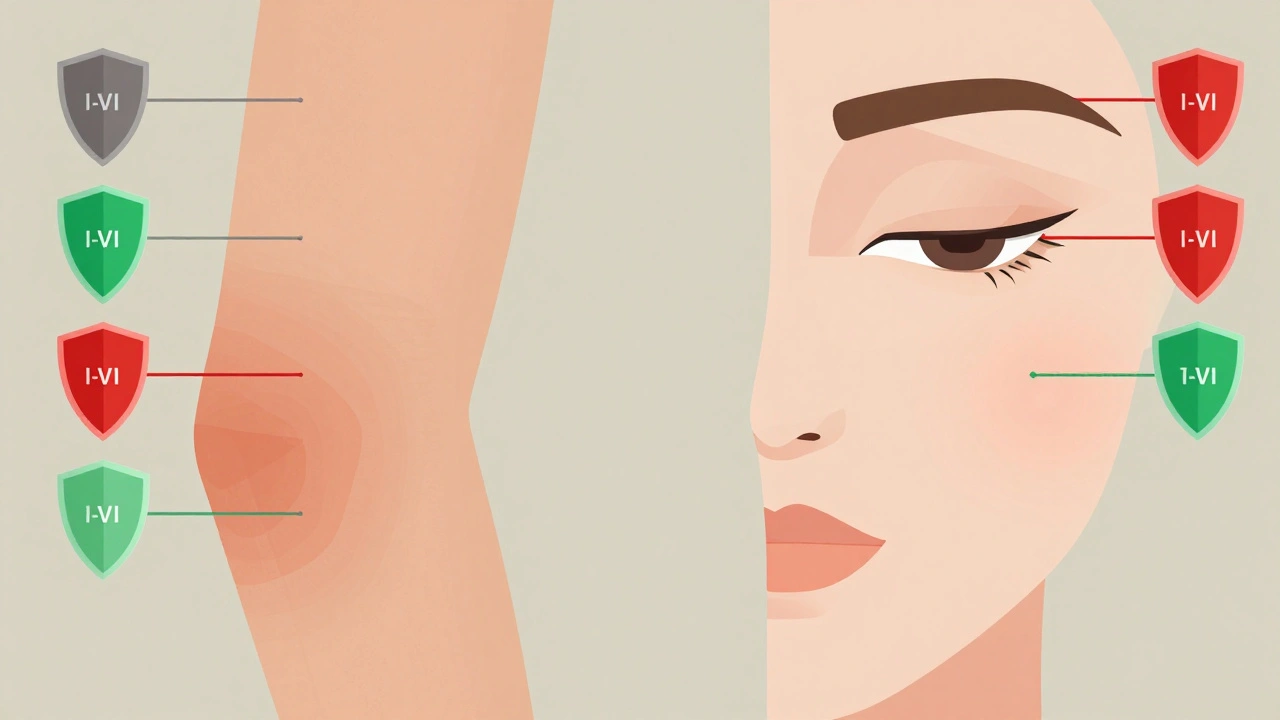
There are seven strength levels, from mild (like 1% hydrocortisone you can buy over the counter) to super-potent (like clobetasol, which needs a prescription). The strength you need depends on your condition, where it is on your body, and how bad the flare is. A rash on your eyelid? Use mild. Thick, scaly patches on your elbows? You might need something stronger.
How Much to Use: The Fingertip Unit Rule
Most people use too little or too much. And both are dangerous.
Doctors measure topical steroid doses in fingertip units (FTUs). One FTU is the amount of cream or ointment you can squeeze from a standard tube onto the tip of your index finger, from the first crease to the tip. It’s not a smear - it’s a line.
One FTU covers an area of skin about the size of two adult hands (front and back). Here’s what you need for common areas:
- One hand (front and back): 1 FTU
- One arm (front and back): 3 FTUs
- One leg (front and back): 6 FTUs
- One foot: 2 FTUs
- Face and neck: 2.5 FTUs total
Using less than this means the treatment won’t work well, and your flare lasts longer - which often leads people to apply more later, increasing side effect risk. Using more than this doesn’t help. It just increases the chance of skin thinning, stretch marks, or acne-like rashes.
Where Not to Use Strong Steroids
Not all skin is the same. The skin on your face, eyelids, groin, armpits, and breasts is thinner and more sensitive. That’s why guidelines are strict:
- Face (including eyelids): Only mild steroids (Class VI-VII), like 1% hydrocortisone. Never use potent or super-potent steroids here unless under direct supervision.
- Genital area: Use only mild to moderate steroids, for no more than 7-14 days.
- Underarms and breasts: Same rules as the groin.
- Palm, soles, elbows, knees: These areas have thick skin. Stronger steroids (Class I-IV) are okay here, even for longer use - but still follow time limits.
Using a strong steroid on your eyelids for weeks can lead to glaucoma or cataracts. Applying it to your inner thighs for months can cause visible skin thinning - the skin becomes see-through, bruises easily, and shows stretch marks. These changes aren’t always reversible.
How Long Is Too Long?
There’s no universal timeline, but here’s what experts agree on:
- Super-potent to potent steroids (Classes I-IV): Use for no more than 2 weeks. If you need more, switch to a weaker one.
- Moderate to low-potency steroids (Classes V-VII): Can be used up to 4 weeks, but only if symptoms haven’t improved in 1-2 weeks, then reassess.
- Never use any topical steroid continuously for more than 4 weeks without seeing a doctor.
Doctors call this the “step-down” approach: start with the strongest steroid that will work, then reduce strength as the skin improves. For example, use clobetasol for 10 days to calm a bad eczema flare, then switch to hydrocortisone for maintenance. This keeps symptoms under control while minimizing risk.
Studies show patients who follow this method rarely develop skin thinning. Those who don’t - especially people self-treating chronic eczema with leftover prescriptions - are the ones ending up with visible damage.
What About Moisturizers?
Moisturizers aren’t optional. They’re part of the treatment. But timing matters.
Apply your steroid first, then wait 20-30 minutes before putting on moisturizer. If you apply moisturizer first, it blocks the steroid from penetrating the skin. If you apply it right after, you dilute it. Either way, you’re wasting the medication.
Also, wash your hands before and after applying. If you touch your eyes, nose, or mouth after handling steroid cream, you can trigger side effects like perioral dermatitis - a red, bumpy rash around the mouth that’s hard to treat.
When You Shouldn’t Use Steroids at All
Topical steroids won’t help infections. If your skin is oozing, crusty, or has pus-filled bumps, you might have a bacterial or fungal infection. Steroids can make these worse by hiding symptoms while letting the infection spread.
Also, avoid using them on broken skin unless directed. Don’t use them for acne - they can cause steroid acne, which looks like tiny red bumps and is hard to clear.
If you’re not sure what’s causing your rash, see a doctor. Don’t guess. A mild steroid might be safe. A strong one on an undiagnosed infection could cause serious damage.
Alternatives When Steroids Are Too Risky
For sensitive areas or long-term use, non-steroidal options exist:
- Calcineurin inhibitors (tacrolimus, pimecrolimus): These are prescription creams that work like steroids but don’t cause skin thinning. Great for face, eyelids, and chronic eczema.
- Crisaborole: A non-steroidal ointment approved for mild-to-moderate eczema in adults and children over 2.
- PDE4 inhibitors: Newer options like ruxolitinib cream, approved for facial and neck eczema.
These are more expensive than steroids and aren’t always covered by insurance. But if you’ve had skin thinning before, or need to treat a sensitive area long-term, they’re worth discussing with your doctor.
What to Do If You Think Your Skin Is Thinning
Signs of skin atrophy include:
- Skin that looks translucent or paper-thin
- Visible blood vessels (telangiectasia)
- Easy bruising
- Stretch marks (striae) that weren’t there before
- Slow healing of cuts or scrapes
If you notice any of these, stop the steroid immediately. Don’t quit cold turkey if you’ve been using it for weeks - talk to your doctor. Abruptly stopping can cause rebound flares. They’ll help you taper off safely.
Thinning skin doesn’t always reverse, but stopping the steroid and protecting the area (with moisturizers and sun protection) can help it stabilize. In some cases, laser treatments or topical retinoids may help improve texture - but only after the steroid is fully out of your system.
Bottom Line: Use Smart, Not Hard
Topical steroids are powerful tools. Used right, they can change your life. Used wrong, they can leave lasting damage. The key isn’t avoiding them - it’s using them with precision.
Follow these three rules:
- Use the weakest steroid that works.
- Apply only the right amount - one FTU per two hand-sized areas.
- Stop after 2-4 weeks, or switch to a milder version.
Don’t rely on advice from social media, old prescriptions, or friends. If your flare keeps coming back, talk to a dermatologist. There’s a better way than just reaching for the strongest tube in your cabinet.
The future of skin care isn’t about avoiding steroids. It’s about using them smarter - with clear instructions, proper timing, and respect for your skin’s limits.
Can topical steroids cause permanent skin thinning?
Yes, especially with long-term use of potent or super-potent steroids on thin skin areas like the face, groin, or armpits. Skin atrophy can become visible and may not fully reverse, even after stopping the medication. Early detection and stopping use can prevent further damage.
How long does it take for skin to recover after stopping steroids?
Recovery varies. Mild thinning may improve over 3-6 months with proper skincare and sun protection. More severe cases can take over a year, and some changes - like visible blood vessels or stretch marks - may be permanent. Avoiding further steroid use and using gentle moisturizers helps the skin heal.
Is hydrocortisone cream safe for daily use?
Over-the-counter 1% hydrocortisone is safe for short-term use (up to 7 days) on small areas. Daily use for more than 2 weeks increases risk of side effects, even with mild steroids. Never use it on the face without a doctor’s advice. For chronic conditions, switch to non-steroidal options after initial flare control.
Why do some people get red rashes after stopping steroid cream?
This is called topical steroid withdrawal (TSW). It happens after prolonged, frequent use - especially on sensitive skin. When you stop, the skin reacts with burning, redness, and flares that can be worse than the original condition. It’s not an allergy - it’s a rebound effect. TSW is rare when steroids are used correctly for short periods. Always taper off under medical supervision.
Can I use steroid cream on my child’s eczema?
Yes, but with extra caution. Children’s skin is thinner and absorbs more. Use only mild to moderate steroids, apply the correct amount (FTUs), and limit use to 7-14 days. Always follow your pediatrician’s or dermatologist’s instructions. Non-steroidal options like tacrolimus are often preferred for long-term use in kids.

amit kuamr
Used clobetasol on my face for two weeks because my acne wouldn’t quit. Now I look like a ghost with veins showing. No regrets? Maybe. But I won’t do it again. Skin doesn’t forgive.