When you’ve been coughing up thick, foul-smelling mucus every day for months-or years-it’s not just a cold that won’t go away. It’s bronchiectasis. This isn’t a simple respiratory bug. It’s a chronic, progressive lung condition where your airways have become permanently widened, scarred, and weak. The result? Mucus builds up, bacteria thrive, and infections keep coming back. The cycle is brutal: infection causes inflammation, inflammation damages the airways, and damaged airways can’t clear mucus, which leads to more infection. And it’s more common than you think. In the U.S., about 350,000 people are diagnosed, but many more go undetected because symptoms creep in slowly, often mistaken for asthma or chronic bronchitis.
What Bronchiectasis Really Feels Like
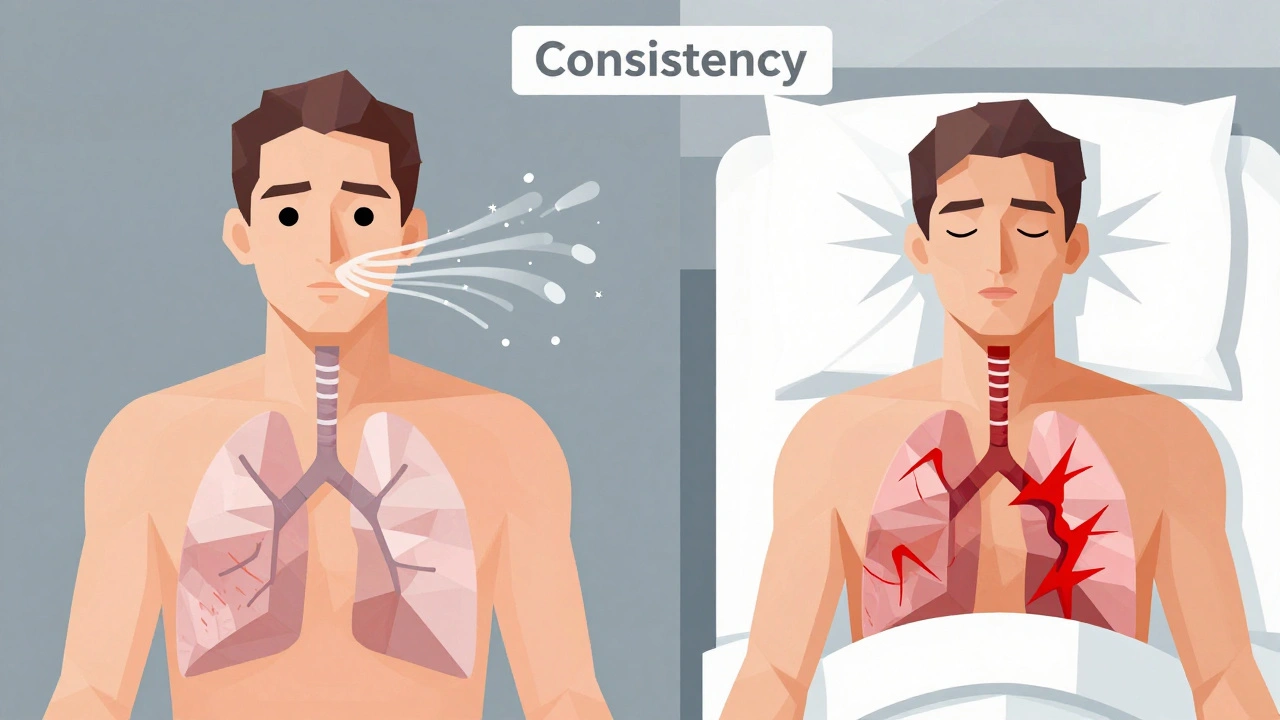
The signature symptom isn’t just a cough-it’s a chronic productive cough that produces at least 30 milliliters of sputum daily. That’s about two tablespoons. The mucus is often yellow or green, sometimes streaked with blood, and has a distinct, unpleasant odor. People describe it as tasting like metal or rotting meat. It doesn’t matter if you’re at work, at the grocery store, or in bed-you feel the need to clear it. And you can’t just swallow it. It has to come out.
Many patients also report shortness of breath, especially after walking up stairs or doing household chores. Fatigue is constant. Some have chest pain that feels like a deep ache, not a sharp stab. Night sweats and weight loss can happen in more advanced cases. But here’s the catch: you might feel fine for weeks, then suddenly get hit with a flare-up-fever, chills, more mucus, worse cough. That’s an exacerbation. And each one chips away at your lung function.
Doctors use CT scans to confirm the diagnosis. The telltale sign? The bronchial artery is at least 1.5 times wider than the pulmonary artery next to it. That’s the gold standard. If you’ve had repeated pneumonia, whooping cough as a child, or immune system issues, your risk goes up. But sometimes, no clear cause is found. That’s called idiopathic bronchiectasis-and it’s surprisingly common.
Why Airway Clearance Isn’t Optional
Here’s the truth most people don’t hear: antibiotics alone won’t fix this. You can take them every time you feel sick, but if the mucus stays stuck, the infection keeps coming back. That’s why airway clearance isn’t just a recommendation-it’s non-negotiable. Dr. Shivani Gupta from Penn Medicine says it plainly: “Daily airway clearance isn’t optional-it’s as essential as taking antibiotics.”
There are several techniques. The most common ones taught by respiratory therapists are:
- Active Cycle of Breathing Techniques (ACBT) - A sequence of breathing control, thoracic expansion exercises, and huff coughing. It’s free, no device needed.
- Positive Expiratory Pressure (PEP) devices - Like the Aerobika®. You breathe out against resistance, which helps push mucus up. Costs $150-$200.
- High-Frequency Chest Wall Oscillation (HFCWO) vests - These vibrate your chest at high speed to loosen mucus. Effective, but expensive-$5,000-$7,000.
- Nebulized hypertonic saline - Breathing in 7% salt water for 10-15 minutes thins mucus so it’s easier to cough up. Often used with dornase alfa.
Studies show that patients who do airway clearance daily have 47% fewer hospitalizations than those who skip it. And their lung function declines slower-only 28 mL per year versus 45 mL for those who don’t stick with it. That’s a huge difference over time.
But learning the technique takes time. Most people need 3-4 one-hour sessions with a therapist. And even then, 55% need a refresher within six months because they’ve forgotten how to do a proper huff cough. A huff isn’t a regular cough. It’s a forced exhalation from different lung volumes-low, medium, high. Do it right, and you feel the mucus move. Do it wrong, and you just get tired.
Antibiotics: The Double-Edged Sword
Antibiotics are the frontline defense against infections. But they’re not a cure. And overusing them creates bigger problems.
For acute flare-ups, doctors usually prescribe a 14-day course of oral antibiotics like amoxicillin-clavulanate or doxycycline. If you’re hospitalized, you might get IV antibiotics like ciprofloxacin or tobramycin.
But for people who have three or more flare-ups a year, long-term antibiotics become necessary. The most common is azithromycin-250 to 500 mg three times a week. This isn’t to treat an active infection. It’s to prevent them. The EMBRACE trial showed this reduces exacerbations by 32% compared to placebo. It works because azithromycin doesn’t just kill bacteria-it also reduces inflammation in the airways.
But here’s the warning: 38% of patients develop antibiotic-resistant bacteria within five years of chronic use. That’s not a small risk. It means the next time you get sick, the usual drugs might not work. That’s why doctors don’t prescribe long-term antibiotics unless you’re having frequent flare-ups and are doing airway clearance consistently.
Inhaled antibiotics like tobramycin (300 mg twice daily) are another option. They target the lungs directly, with fewer side effects than pills. They’re especially helpful if you have Pseudomonas aeruginosa in your sputum-a tough bug that loves bronchiectasis airways. Studies show they cut Pseudomonas colonization by 56%.
The FDA approved a new inhaled treatment called gallium maltolate in 2023 for stubborn Pseudomonas infections. Early results show a 42% drop in flare-ups. That’s promising, but it’s still reserved for cases where other treatments have failed.
What Doesn’t Work (and Why)
Not every treatment helps everyone. Bronchodilators-like albuterol inhalers-are often prescribed, but they only improve symptoms by 12% on their own. They’re not magic. But when combined with airway clearance, symptom relief jumps to 28%. So if you’re using an inhaler, make sure you’re pairing it with clearing your airways.
Some people try herbal remedies, steam inhalation, or chest rubs. These might feel good temporarily, but they don’t remove mucus. And if you skip the science-backed methods because “it feels better,” you’re risking long-term damage.
And don’t wait for symptoms to get bad before acting. The European Respiratory Society warns that patients who only take antibiotics during flare-ups have 2.3 times higher risk of permanent lung function decline. Prevention is everything.
The Real Cost-Time, Money, and Mental Load
Bronchiectasis doesn’t just cost money-it costs time. Daily airway clearance takes 15 to 45 minutes, depending on your regimen. Add in nebulizer treatments, medication schedules, and doctor visits, and you’re looking at over an hour a day. For someone working two jobs or raising kids, that’s overwhelming.
Annual healthcare costs average $18,500 per person in the U.S. Most of that goes to hospitalizations ($8,700) and antibiotics ($6,200). Insurance often covers antibiotics and nebulizers, but not always the devices. An Aerobika® costs $150-$200. Many patients say insurance won’t pay unless you prove you’ve tried cheaper options first. That’s a barrier.
And then there’s the emotional toll. On online forums like Reddit’s r/Bronchiectasis and the American Lung Association’s community, people talk about feeling isolated. One patient wrote: “I canceled plans because I was too tired. Then I felt guilty. Then I coughed in front of my kids and they got scared.”
Support groups help. The Bronchiectasis and NTM Initiative runs monthly virtual meetings with over 120 participants. There’s also a free app called “Clearing the Air” from the American Thoracic Society that lets you log your daily clearance, track symptoms, and get reminders. It’s not fancy, but it works.

What’s Next? Hope on the Horizon
Research is moving fast. A new registry launched in 2022 has tracked 5,000 patients across 75 centers. They’ve found genetic markers that predict who’s likely to decline faster. That means in the next few years, treatment could be personalized-not just based on symptoms, but on your DNA.
Another exciting area: bacteriophages. These are viruses that target specific bacteria. Dr. James Chalmers in Scotland is testing inhaled phages for antibiotic-resistant Pseudomonas. Early data shows 68% of patients cleared the infection. If this works, it could be a game-changer for people who’ve run out of antibiotic options.
But the biggest challenge isn’t science-it’s access. Medicaid patients have 3.2 times more flare-ups than those with private insurance. Why? They can’t get regular respiratory therapy. They can’t afford devices. They live in areas without specialists. Until we fix that, bronchiectasis will keep being a disease of inequality.
How to Start Today
If you’ve been diagnosed:
- Find a respiratory therapist. Ask your pulmonologist for a referral.
- Learn ACBT or get an Aerobika® device. Start with 15 minutes, twice a day.
- Drink at least 2 liters of water daily. Hydration thins mucus.
- Use 7% hypertonic saline nebulizer if prescribed. Don’t skip it.
- Keep a symptom journal. Note cough frequency, mucus color, energy levels.
- Get the flu shot and pneumococcal vaccine every year.
- Don’t wait for a flare-up to call your doctor. If you feel worse for more than 48 hours, act.
If you haven’t been diagnosed but have a daily cough with thick mucus for over 8 weeks:
- Don’t brush it off as “just a smoker’s cough” or “post-nasal drip.”
- Ask your doctor for a chest CT scan. That’s the only way to confirm bronchiectasis.
- Bring a sample of your sputum if you can. Color and smell matter.
Bronchiectasis isn’t a death sentence. But it demands discipline. It’s not about being perfect. It’s about showing up every day-even when you’re tired, even when you’re frustrated. Because every cleared airway, every avoided infection, every day of consistent care adds up to more years of breathing easy.
Can bronchiectasis be cured?
No, bronchiectasis cannot be cured because the airway damage is permanent. But with consistent airway clearance, appropriate antibiotics, and lifestyle management, progression can be slowed significantly, symptoms can be controlled, and quality of life can improve dramatically. Many people live full, active lives with proper care.
How do I know if I’m doing airway clearance right?
You’ll know you’re doing it right when you feel mucus move and can cough it up more easily. If you’re using a PEP device, you should feel resistance when exhaling, and your chest should feel looser afterward. If you’re doing ACBT, you should hear or feel a change in your cough from shallow to deeper. A respiratory therapist can observe your technique and give feedback. Most people need at least 12 supervised sessions to get it right.
Why do I need to take antibiotics if I don’t feel sick?
Long-term antibiotics like azithromycin aren’t meant to treat an active infection-they’re for prevention. They reduce inflammation in the airways and lower the chance of bacteria taking hold. If you only take them when you’re sick, the infection keeps coming back, and your lungs get more damaged over time. Studies show daily preventive antibiotics cut flare-ups by over 30%.
Is it safe to use hypertonic saline long-term?
Yes. Nebulized 7% hypertonic saline is safe for daily use and is widely recommended by major respiratory societies. It draws water into the airways, thinning mucus so it’s easier to clear. Some people experience mild coughing or throat irritation at first, but that usually improves after a few days. Always use sterile saline made for nebulizers-never homemade salt water.
What happens if I stop airway clearance?
If you stop daily airway clearance, mucus builds up again. Bacteria multiply. Infections return faster and stronger. Within months, you’ll likely see your cough worsen, your energy drop, and your lung function decline faster-up to 45 mL per year instead of 28 mL. You’ll also be more likely to end up in the hospital. Consistency is the single biggest factor in preventing long-term damage.
Can I exercise with bronchiectasis?
Yes-exercise is encouraged. Regular physical activity helps loosen mucus, improves breathing efficiency, and boosts overall health. Walking, swimming, and cycling are great. Avoid high-intensity workouts if you’re having a flare-up. Always do airway clearance before and after exercise. Many patients report better symptom control and more stamina after starting a consistent routine.


Vivian Amadi
This post is literally the only thing that made sense about my diagnosis. Everyone else just says 'drink water' like it's a magic spell. I've been doing ACBT for 8 months and my sputum volume dropped 60%. If you're not doing it daily, you're just delaying the inevitable hospital trip. Stop pretending this is optional.