Every year, thousands of children receive the wrong dose of medicine because of a simple mistake: a weight calculation gone wrong. It doesn’t take much - a misplaced decimal, a conversion from pounds to kilograms, or an outdated weight on the chart. These aren’t theoretical risks. They’re real, preventable errors that land kids in the hospital instead of helping them get better. The solution isn’t more training or better memory. It’s a system - one built around accurate, verified, weight-based checks at every step of the process.
Why Weight Is the Key to Pediatric Dosing
Children aren’t just small adults. Their bodies process drugs differently. A dose that’s safe for a teenager could be deadly for a 6-month-old. That’s why nearly all pediatric medications are dosed by weight - milligrams per kilogram (mg/kg) or sometimes per square meter of body surface area. This means the exact weight of the child becomes the most important number in the entire prescription process.But here’s the problem: weight isn’t always accurate. A child might have been weighed months ago. The scale might have been set to pounds instead of kilograms. A parent might have guessed the weight. Or worse, the weight might be entered correctly but forgotten during a busy shift. According to the World Health Organization, children are three times more likely to suffer a medication error than adults. And nearly one in five of those errors come from weight-related miscalculations.
Take liquid antibiotics, for example. If a 10-kilogram child needs 10 mg/kg of amoxicillin, they need 100 mg total. If the concentration is 250 mg/5 mL, that’s 2 mL. But if the weight is misread as 100 kg instead of 10 kg? That’s 100 times too much. That’s not a typo. That’s a medical emergency.
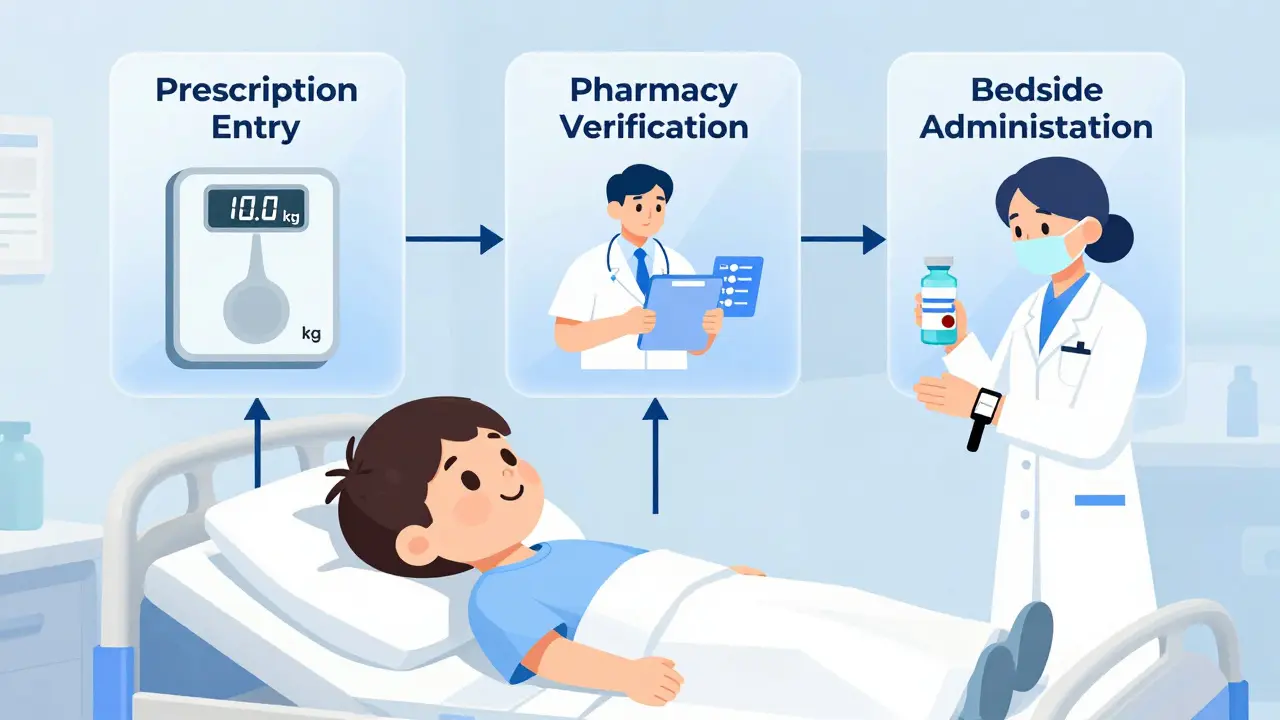
The Three Points of Weight Verification
The most effective way to stop these errors isn’t to rely on one person to catch a mistake. It’s to build checks into the system - at three critical points:- Prescription entry - The provider must enter the child’s current weight before the order can be submitted.
- Pharmacy verification - The pharmacist must independently confirm the weight and recalculate the dose before dispensing.
- Bedside administration - The nurse must check the weight again when giving the medication, matching it to the label.
This isn’t just theory. Dr. Matthew Grissinger of the Institute for Safe Medication Practices calls this the gold standard. And the data backs it up. A 2022 study from Boston Children’s Hospital showed that after implementing this three-point check, weight-related dosing errors dropped from 14.3 per 10,000 doses to just 0.8. That’s a 94% reduction.
But it only works if each step is mandatory, not optional. If a provider can skip entering weight to save time, they will. If a pharmacist can override a warning without logging why, errors will slip through. Systems must be designed to force action - not just suggest it.
Technology That Works - And What Doesn’t
Technology can help, but not all of it does. Electronic health record (EHR) systems with built-in clinical decision support can cut dosing errors by up to 87%. But only if they’re configured right.Here’s what works:
- Kilograms only - No pounds. No stones. No guesswork. Systems should require weight entry in kilograms only. This alone cuts out 12.6% of all conversion errors.
- Automatic calculations - The system should auto-calculate the dose based on weight and standard concentrations. No manual math.
- Upper and lower limits - If a dose is too high or too low for the child’s weight, the system should block the order and require a second review.
- Barcode matching - When the nurse gives the medicine, scanning the child’s wristband and the medication should cross-check the weight and dose. Studies show this reduces errors by 74%.
What doesn’t work? Paper-based systems. Preprinted charts with dosing tables. They’re outdated. A 2019 study found they only reduce errors by 36.5% - less than half the effectiveness of computerized systems.
Even smart systems can fail if they’re not tuned to the real world. For example, some EHRs flag adolescent doses as “too high” because they’re programmed for younger kids. Pharmacists on Reddit report being flooded with false alerts for teens near adult weight ranges. That leads to alert fatigue - where clinicians start ignoring warnings altogether. A 2021 study found that 41.7% of weight-based alerts were overridden, and nearly one in five of those overrides were actual errors.
That’s why newer systems like Epic’s Pediatric Safety Module 4.0 (released in January 2024) use growth percentiles instead of fixed weight limits. If a child’s weight is in the 85th percentile for their age, the system adjusts the safe dose range accordingly. This cut inappropriate alerts by 63% in testing.

The Hidden Problem: Outdated Weights
Even the best system can’t help if the weight is wrong from the start.A 2022 survey of 1,247 pediatric nurses found that 63.2% had seen incorrect weight documentation in the past year. In 41.7% of those cases, it caused delays in giving medication - or worse, gave the wrong dose. The Institute for Safe Medication Practices says this is one of the biggest overlooked risks. Their 2023 guidelines say: “Weight-based verification systems fail when patient weights are outdated.”
That’s why hospitals now require:
- Weight measured within 24 hours for kids in acute care (ER, ICU, inpatient).
- Weight updated every 30 days for outpatient visits.
- Re-weighing before surgery or high-risk procedures, even if weight was recent.
And the scales? They must show only kilograms. The American Academy of Pediatrics recommends digital scales with 0.1 kg precision for infants and 0.5 kg for older children. No rounding. No guesswork.
Standardizing Concentrations Saves Lives
Another hidden source of error? Variable drug concentrations.Imagine two different vials of vancomycin. One is 5 mg/mL. Another is 10 mg/mL. A pharmacist calculates the dose for the first, but the nurse grabs the second. Suddenly, the child gets twice the medicine. This isn’t rare. A 2023 study found that facilities using standardized concentrations - like always using 5 mg/mL for common antibiotics - reduced calculation errors by 72.4%.
That’s why top hospitals now lock down concentrations. No exceptions. No “just this once.” If a drug has multiple concentrations, it’s either discontinued or replaced with a single, approved version.

Training, Culture, and the Human Factor
Technology can’t fix everything. You still need trained staff who understand pediatric pharmacokinetics. A 2022 survey found that 37.8% of pharmacy staff lacked adequate training in how children metabolize drugs.Successful programs don’t just train once. They require:
- 40 hours of initial training for all clinicians.
- Quarterly competency checks with 90% accuracy required to keep practicing.
- Non-punitive reporting - if someone catches a near-miss, they’re praised, not punished.
And staffing matters. Dr. Kate Wang’s research shows that for every 100 pediatric beds, you need 2.5 full-time pharmacists dedicated to verification. Without that, the system collapses under workload.
But the biggest cultural shift? Making weight verification non-negotiable. Not a suggestion. Not an option. A rule - like wearing gloves or washing hands. If a child’s weight isn’t confirmed, no drug leaves the pharmacy. No nurse gives the dose. No order gets filled. That’s how safety becomes routine.
The Bigger Picture: Access and Equity
Here’s the uncomfortable truth: not all hospitals can afford this.While 94% of academic children’s hospitals have full weight-based systems, only 32.7% of rural community hospitals do. That’s a massive gap. Kids in rural areas are more likely to get the wrong dose because they lack EHR integration, trained pharmacists, or even reliable scales.
Regulatory pressure is starting to change that. The Leapfrog Group now requires weight verification for hospitals to earn an “A” safety rating. Medicare and Medicaid now require weight documentation for all pediatric prescriptions. The market for pediatric safety tech is projected to hit $2.3 billion by 2027.
But progress won’t be fair unless we invest in the places that need it most. Simple solutions - like downloadable weight calculators, standardized paper dosing charts, and mobile apps that auto-convert pounds to kilograms - can help smaller clinics bridge the gap.
What Families Can Do
Even with the best systems, parents are the last line of defense.Ask these three questions before your child takes any new medication:
- “What is my child’s weight in kilograms?” - If they say pounds, ask them to convert it.
- “Can you show me how you calculated the dose?” - Don’t be shy. You have the right to understand.
- “Is this dose in milliliters? Not teaspoons or tablespoons?” - The American Academy of Pediatrics says liquid meds should only be labeled in mL. Anything else is outdated.
If something feels off - trust your gut. Speak up. It’s not rude. It’s lifesaving.
Why do pediatric medications use weight instead of age?
Age is a rough guide, but weight is the real factor. A 2-year-old weighing 15 kg may need the same dose as a 5-year-old weighing 15 kg - even if their ages are different. Children’s bodies absorb, metabolize, and eliminate drugs based on their size, not their birthday. Weight-based dosing ensures the dose matches the child’s actual physiology, not a general rule of thumb.
Can’t pharmacists just double-check the dose manually?
Manual checks help, but they’re not enough. Humans make calculation errors - especially under pressure. A 2020 study showed that even experienced pharmacists made mistakes in 12% of manual weight-based calculations. Automated systems that calculate the dose from the entered weight cut that error rate to under 2%. Manual checks should be a backup, not the main safety layer.
What if a child’s weight changes quickly - like after surgery or fluid shifts?
In acute care settings, weight should be re-measured every 24 hours - or even more often if the child is losing or gaining fluid rapidly. For example, a child with severe dehydration might gain 2 kg after IV fluids. If the dose was calculated before the fluid shift, it could be dangerously low. That’s why hospitals use real-time weight updates, not static chart entries.
Do all liquid medications need to be labeled in milliliters?
Yes. The American Academy of Pediatrics requires all pediatric liquid medications to be labeled in milliliters (mL) only. Teaspoons, tablespoons, or drops are outdated and dangerous. A teaspoon can vary from 4-6 mL depending on the spoon. Using mL ensures precision. If you see a dose written as “1 tsp,” ask for it to be rewritten in mL.
How can rural clinics implement weight-based checks without expensive tech?
Start simple. Use standardized dosing charts printed in kilograms. Train staff to always weigh in kg. Use free online calculators that auto-convert pounds to kg. Pair pharmacists with nurses for dual verification. Even without EHRs, a checklist and culture of double-checking can cut errors by 50% or more. The goal isn’t perfection - it’s consistency.

Jonathan Noe
This is literally the most important thing no one talks about. I work in ER pediatrics and saw a kid almost die because someone used pounds instead of kgs. The system didn't flag it because the weight was 'plausible' - 150 lbs entered as 150 kg. One decimal. One mistake. One near-tragedy. We need mandatory kg-only entry. Period.