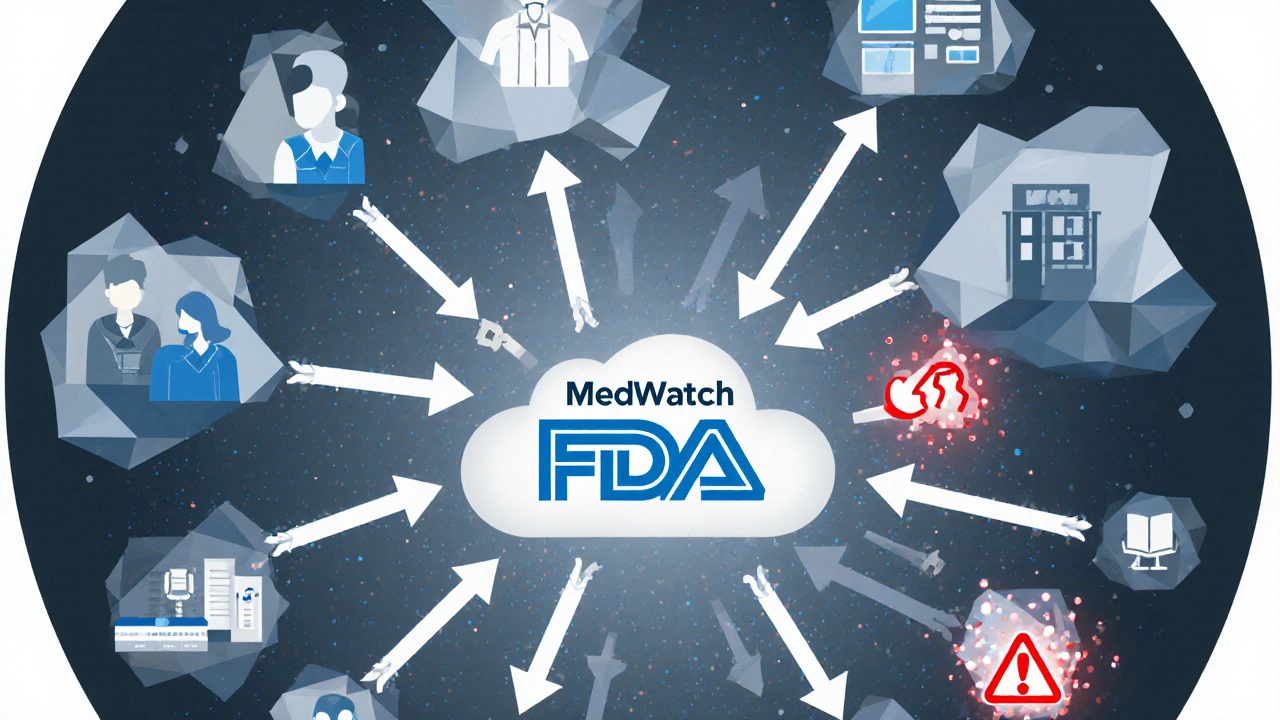
The U.S. Food and Drug Administration doesn’t just approve drugs and medical devices-it watches them after they’re in your hands. That’s where MedWatch comes in. It’s not a flashy app or a high-tech gadget. It’s a quiet, behind-the-scenes system that collects reports of harm caused by medications, implants, vaccines, and even cosmetics. And without it, we’d be flying blind when something goes wrong.
What Exactly Is MedWatch?
MedWatch, officially called the FDA Safety Information and Adverse Event Reporting Program, is the FDA’s main tool for tracking problems with medical products after they hit the market. Launched in 1993, it was created because the agency realized that clinical trials-no matter how thorough-can’t catch every possible side effect. Some reactions only show up when thousands or millions of people use a drug over time. MedWatch fills that gap. It doesn’t just collect data. It also sends out alerts. If a new risk is spotted-like a heart rhythm issue linked to a common antibiotic or a device that breaks inside the body-the FDA uses MedWatch reports to warn doctors and patients. You can find these alerts on the MedWatch website, in email updates, or through RSS feeds. The system covers a wide range of products: prescription and over-the-counter medicines, biologics like insulin or monoclonal antibodies, medical devices (from pacemakers to glucose monitors), combination products (like pre-filled syringes), and even hemp-based products and cosmetics. If it’s regulated by the FDA and something bad happens, MedWatch is where it gets reported.Who Reports to MedWatch?
There are two kinds of reporters: those who have to report, and those who can report. Manufacturers, importers, and hospitals that use medical devices are legally required to file reports using Form FDA 3500B. If a device causes a death or serious injury, they have to notify the FDA within 30 days-or within five workdays if it’s a life-threatening situation. Drug companies must report serious side effects too. Failure to report can mean fines or legal action. But the real power of MedWatch comes from the people who aren’t required to report: you. Healthcare professionals-doctors, nurses, pharmacists-and everyday consumers can submit voluntary reports using Form FDA 3500. In 2022, 42% of all reports came from patients or family members, not professionals. That’s huge. It means the system relies on people noticing something unusual and speaking up.How Does a Report Turn Into Action?
Every year, about 1.2 million reports flow into MedWatch. Most go into the FDA Adverse Event Reporting System (FAERS), a massive database holding over 28 million records. But raw data doesn’t tell you much. The real work starts when analysts look for patterns. They use statistical tools like the Proportional Reporting Ratio (PRR) and Bayesian Confidence Propagation Neural Network (BCPNN) to spot unusual spikes. For example, if 500 people report sudden liver damage after taking a new diabetes drug, but only 2 people reported the same with older drugs, that’s a red flag. The FDA’s Division of Pharmacovigilance reviews about 5,000 potential signals each year. If the pattern holds up, they dig deeper. They might review medical records, contact the reporting doctor, or check other global databases. If the risk is confirmed, they can do things like:- Update the drug’s warning label
- Require a Risk Evaluation and Mitigation Strategy (REMS)
- Limit who can use the product
- Issue a public safety alert
- Recall the product
What Makes a Good Report?
Not every report helps. If you report that you felt dizzy after taking a pill, but don’t say which pill, when you took it, or how long the dizziness lasted-it’s useless. The FDA says a good report includes:- The name of the product (drug, device, or biologic)
- Exact brand and generic names
- NDC code for drugs or model number for devices
- Patient’s age and sex (if known)
- When the problem started after using the product
- What happened (symptoms, test results, hospitalization)
- Any other medicines or conditions the patient has
- What was done to treat it
- What the outcome was (recovered, disabled, died)
Why Do So Few People Report?
Despite its importance, experts agree: MedWatch is underused. Studies estimate only 1% to 10% of actual adverse events are reported. Why? For patients, it’s confusing. A 2022 survey by the National Consumers League found 68% of people struggled with medical terms. One woman tried to report her husband’s reaction to a blood thinner but gave up because she didn’t know how to describe the bleeding. For doctors, it’s time. The American Medical Association found it takes 15-20 minutes to file a full report. That’s a lot when you’re already running behind. But if your electronic health record (EHR) is linked to MedWatch-like Epic Systems-it drops to 8-12 minutes. Only about 35% of providers have that integration. And then there’s the mindset. Many think, “It’s probably just a coincidence.” Or, “Someone else will report it.” But if no one reports, the FDA can’t see the problem.
What’s New in MedWatch?
The system isn’t stuck in 1993. In September 2023, the FDA launched MedWatch Direct-a new API-based system that lets EHRs and pharmacy software send reports automatically. Think of it like your phone updating apps in the background. If your doctor’s system detects a serious reaction, it can notify the FDA without you lifting a finger. By mid-2024, the FDA plans to use AI to scan clinical notes for signs of adverse events. Right now, a human reads each report. In the future, AI might flag patterns from thousands of doctor’s notes, speeding up detection. They’re also testing blockchain to verify report authenticity and reduce fake submissions. And funding is rising: $47.8 million in FY2024, up 12% from last year. But challenges remain. Only 120 full-time staff analyze over a million reports annually. That’s less than 10,000 reports per person. No amount of AI can fix underreporting.How to File a Report
It’s free, and you don’t need to be a doctor. Here’s how:- Go to www.fda.gov/medwatch
- Click “Report a Problem”
- Choose your role: healthcare professional, consumer, or manufacturer
- Fill out Form FDA 3500 online
- Or download the PDF, fill it out, and mail or fax it
Is MedWatch Effective?
Yes-but not perfect. Between 2015 and 2020, MedWatch reports contributed to 37% of all FDA safety communications. That’s nearly four in ten warnings you’ve seen on drug labels or news alerts started with a patient or doctor’s report. But Dr. Joel Lexchin from York University calls it “a system with holes.” He’s right. If only 1% of problems are reported, the FDA is working with a distorted picture. That’s why experts push for better tools, better education, and better integration into clinical workflows. The bottom line: MedWatch is the most important safety net we have for drugs and devices. It’s not glamorous. It doesn’t make headlines. But when it works, it saves lives.Is MedWatch only for prescription drugs?
No. MedWatch accepts reports for prescription drugs, over-the-counter medicines, vaccines, medical devices (like pacemakers or insulin pumps), biologics, combination products, hemp-based products, and even cosmetics. If the FDA regulates it and something bad happened, it’s reportable.
Do I need to prove the product caused the problem to report it?
No. You don’t have to be certain. The FDA just needs to know something unusual happened after using the product. Even if you think it’s a coincidence, report it. Patterns emerge from many reports-not one.
Can I report an adverse event for someone else?
Yes. Family members, caregivers, or friends can file a report on behalf of a patient. Just include as much information as you can about the person, the product, and what happened.
How long does it take for the FDA to act after a report?
It varies. For urgent safety issues-like a life-threatening reaction-the FDA can issue a warning in days. For slower-developing patterns, analysis can take months. The key is volume: one report won’t trigger action, but 50 similar ones might.
Are MedWatch reports anonymous?
You can choose to remain anonymous. But providing your contact info helps the FDA follow up if they need more details. Your information is protected under privacy laws and won’t be shared publicly.
What if I don’t know the product’s NDC code or model number?
Try checking the packaging, prescription label, or receipt. If you can’t find it, describe the product as clearly as possible-brand name, color, shape, size, or where you bought it. The FDA can often identify it from your description.

Scott Walker
This is actually really cool. I had no idea regular folks could report side effects. Kinda makes you feel like you’re part of the system, ya know? 👍