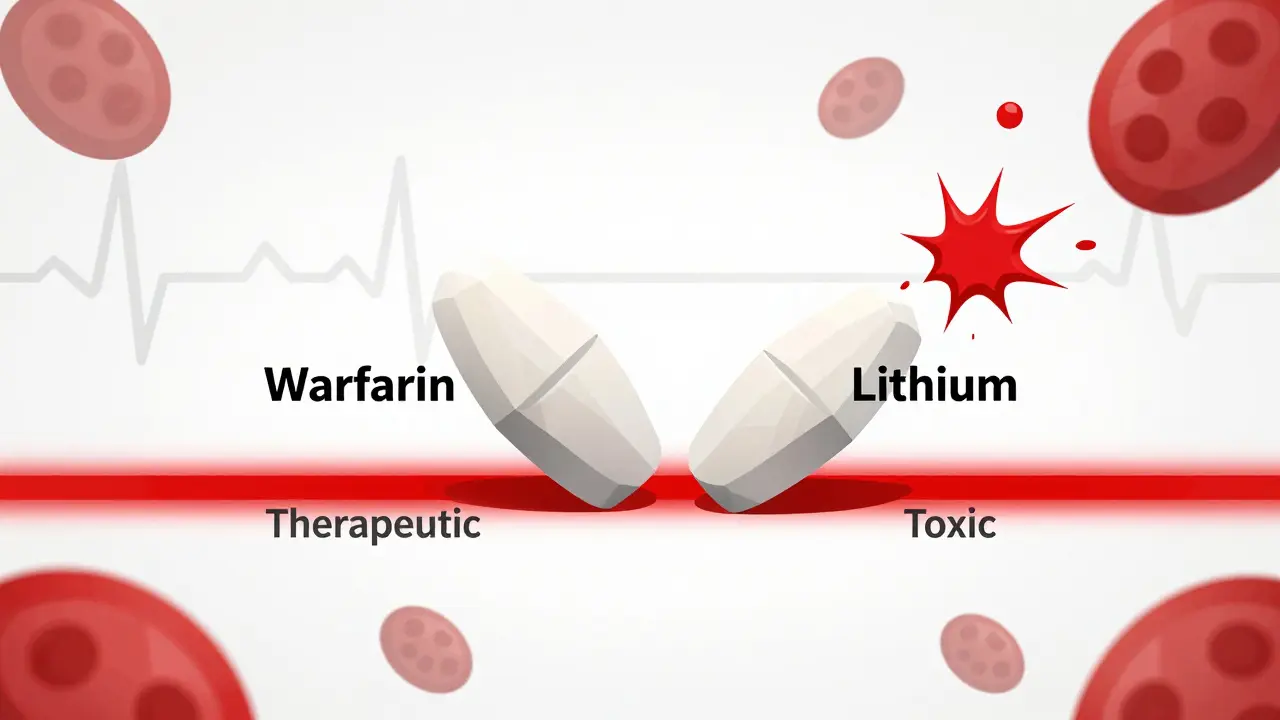
When you’re on a combination of NTI drugs, even a tiny change in dosage can mean the difference between healing and hospitalization. These are not your average medications. NTI stands for Narrow Therapeutic Index - meaning the gap between a dose that works and one that harms is razor-thin. Warfarin, lithium, levothyroxine, phenytoin - these drugs save lives, but they demand precision. Now imagine taking two of them together in a single pill. That’s where things get dangerous, especially when generics enter the picture.
What Makes NTI Drugs So Risky?
NTI drugs have a very small window between effectiveness and toxicity. For example, warfarin’s blood level needs to stay within a range of just 2 to 3 mg/L. Go slightly above that, and you risk internal bleeding. Go slightly below, and a blood clot could form. The FDA defines NTI drugs by five key traits: minimal safety margin, high risk of life-threatening side effects, need for frequent blood tests, low variation in how your body processes them, and the need for frequent small dose tweaks.
These aren’t just theoretical concerns. In 2015, a Harvard study found that 18.7% of patients on generic warfarin had unstable INR levels - a measure of blood clotting - compared to just 4.3% on the brand version. That’s a fourfold increase in risk. And when you combine two NTI drugs? The risk doesn’t just add up - it multiplies.
Why Combination NTI Drugs Are Rarely Generic
There are over 100 FDA-approved NTI drugs. Most have generic versions. But when it comes to fixed-dose combinations - pills that contain two or more NTI drugs in one tablet - the market is nearly empty. Why?
It’s not about cost. It’s about science. The FDA requires generic drugs to prove they’re bioequivalent to the brand - meaning they deliver the same amount of drug into the bloodstream at the same rate. For regular drugs, that’s 80% to 125% similarity. For NTI drugs, it’s tighter: 90% to 111% for peak levels (Cmax) and 90% to 112% for total exposure (AUC).
Now imagine a pill with two NTI drugs. Each one has to hit that narrow window - independently. If Drug A is at 108% and Drug B is at 109%, the combined effect isn’t just 217%. It’s unpredictable. One drug might push your INR too high, while the other barely reaches therapeutic levels. The math doesn’t work.
As of October 2023, the FDA Orange Book listed 11 approved generic versions of warfarin. But zero fixed-dose combinations containing warfarin and another NTI drug. Same with lithium and valproate. Same with digoxin and amiodarone. No approved products. No generics. Not one.
The Real-World Cost of the Gap
Patients on combination NTI therapy are stuck. They either pay high brand prices - sometimes over $300 a month - or risk switching to separate generics. But even that’s risky. A 2020 JAMA study showed patients on combination regimens with one NTI drug had a 27% higher chance of adverse events after generic substitution than those on non-NTI combinations.
One patient on Reddit shared: “After my pharmacy switched my generic warfarin, my INR jumped from 2.5 to 6.8 in three days. I ended up in the ER. Now I’m on brand. I can’t afford it, but I won’t risk it again.”
Pharmacists see this daily. A 2023 ASHP survey of 856 pharmacists found that 78.3% had witnessed therapeutic failure after generic substitution in NTI combinations. Over 40% reported serious adverse events - hospitalizations, bleeding, seizures.
And it’s not just about safety. Monitoring costs skyrocket. Patients on combination NTI therapy need blood tests every 2-4 weeks. That’s $1,200 to $2,500 a year just for lab work. For non-NTI combinations, it’s under $800. Add in doctor visits, dose adjustments, and time off work - the hidden cost is massive.

Why Manufacturers Won’t Try (And Why Some Say They Should)
Generic drugmakers like Teva and Sandoz have the technology to make precise pills. In Europe, some generic combinations of levothyroxine and selenium have been used safely since 2015, with under 2% adverse events. But the U.S. system demands more. The FDA’s 2022 standards were already tough. In February 2023, they proposed even tighter rules for combination NTI drugs: 90% to 107.69% for Cmax and 90% to 110% for AUC. That’s a 17.69% window for one drug - and both drugs must hit it simultaneously.
Dr. Donald Berry, a biostatistician at MD Anderson, put it bluntly: “The 90-111% window still allows 22% total variation. When you combine two NTI drugs, that’s a 44% swing in overall effect. That’s not bioequivalence - that’s chaos.”
Some argue the standards are too strict. Others say they’re not strict enough. The truth? We don’t have the tools to measure what really matters in combination therapy: how the drugs interact in real people over time.
What’s Being Done - And What’s Not
The FDA is working on a 2024 pilot program called “precision bioequivalence.” It uses computer modeling to predict how combinations behave in the body - instead of just testing blood levels in 24 healthy volunteers. That’s a start. But it’s still experimental. And it won’t help the 12,000 Americans currently on combination NTI therapy who can’t afford brand-name drugs.
Meanwhile, enterprise hospitals have already taken action. A 2023 ASHP report found that 87% of large hospital systems block automatic substitution of NTI-containing combinations. Community pharmacies? Only 27% do. That means a patient walking into a CVS might get switched to generics - while their oncologist or cardiologist is screaming in the background.
Documentation is another mess. FDA-approved NTI monotherapy labels average a 4.2 out of 5 for clarity. Combination NTI labels? 2.8. That’s not just confusing - it’s dangerous.

Where Do We Go From Here?
There’s no easy fix. But here’s what needs to happen:
- Stop automatic substitution. Pharmacists should never switch a combination NTI drug without a doctor’s explicit approval.
- Require special labeling. All combination NTI drugs - brand or generic - should carry a black box warning: “Do not substitute without clinical supervision.”
- Invest in real-world data. We need registries tracking patients on these regimens. Not just lab numbers - hospitalizations, quality of life, cost of care.
- Reform reimbursement. Medicare and insurers should cover brand-name combinations for patients who need them - not force them to gamble with generics.
The NTI drug market is worth nearly $50 billion. But less than 0.3% of that is combination therapy. That’s not because no one needs it. It’s because we haven’t figured out how to make it safe.
Patients aren’t asking for cheaper drugs. They’re asking for reliable ones. And until we can guarantee that two narrow-window drugs behave predictably together - we’re not just failing them. We’re putting them at risk.
Are there any generic combination NTI drugs available in the U.S.?
No. As of 2023, there are no FDA-approved fixed-dose combination products containing two or more NTI drugs on the U.S. market. While single-agent NTI drugs like warfarin or levothyroxine have many generic versions, the bioequivalence requirements for combinations are currently impossible to meet under existing FDA standards. The FDA Orange Book shows zero approved combination NTI generics.
Why can’t generic manufacturers just make combination NTI drugs?
It’s not a manufacturing issue - it’s a science issue. Even if a generic company makes two perfectly precise NTI drugs, combining them into one pill creates unpredictable interactions. The FDA requires each component to stay within a 90-111% bioequivalence window. When two drugs are combined, their variations multiply. A 10% rise in one drug plus a 10% rise in another doesn’t equal 20% - it can cause a dangerous spike in blood levels or therapeutic failure. No current testing method can reliably predict this in real patients.
Is it safe to switch from brand to generic for NTI drugs?
For single-agent NTI drugs, switching carries risk - and should only be done under close medical supervision. Studies show 18-27% of patients experience instability after switching. For combination NTI drugs, switching is not recommended. The American Society of Health-System Pharmacists (ASHP) explicitly opposes automatic substitution in these cases. If you’re on a combination, ask your doctor to prescribe the exact brand you’re on - and never let your pharmacy substitute without approval.
How often do patients need blood tests on combination NTI therapy?
Patients on combination NTI therapy typically need blood tests every 2 to 4 weeks during initial stabilization - that’s 12 to 26 tests in the first three months. Once stable, testing may drop to every 4 to 8 weeks. This is far more frequent than for non-NTI combinations, which usually require testing every 8 to 12 weeks. Annual testing costs average $1,200 to $2,500 per patient.
What’s the difference between NTI and regular combination drugs?
Regular combination drugs, like entecavir/tenofovir for HIV, have wide safety margins. Even if blood levels vary by 20%, it doesn’t cause harm. NTI combinations - like warfarin + amiodarone - have no safety buffer. A 10% change in either drug can trigger bleeding, arrhythmia, or organ failure. That’s why generic versions of non-NTI combinations are common, but NTI combinations are almost nonexistent.
Can I ask my doctor to prescribe only brand-name combination NTI drugs?
Yes - and you should. If you’re on a combination therapy involving NTI drugs, ask your prescriber to write “Dispense as Written” or “Do Not Substitute” on the prescription. Many insurers will cover the brand if you can prove medical necessity. Some states require pharmacies to notify you before switching. Know your rights - and don’t let cost override safety.
Final Thoughts
The system is built to save money - but it’s costing lives. We have generics for almost every NTI drug. But when patients need more than one, we leave them behind. There’s no technical reason we can’t make safe combination NTI generics. But there’s a regulatory, financial, and cultural reason we haven’t tried hard enough.
Patients deserve more than a gamble. They deserve predictable, reliable treatment. Until we fix the rules, the only solution is vigilance: know your drugs, demand clear prescriptions, and never accept a switch without talking to your doctor first.

Hanna Spittel
This is all just Big Pharma playing us. 🤡 They don't want generics because they're scared someone will figure out the real formula... and then we'd all be free. 💊🔥