When a patient walks into your pharmacy or clinic and sees their prescription has switched from a brand-name pill to a generic, they often don’t ask if it’s the same. They just stare at the new color, size, or shape-and worry. Generic medications are not second-rate. They’re the same medicine, approved by the FDA, with the same active ingredient, strength, and effect. But if you don’t explain that clearly, patients will assume something’s wrong. And that’s where adherence falls apart.
Why Patients Doubt Generics
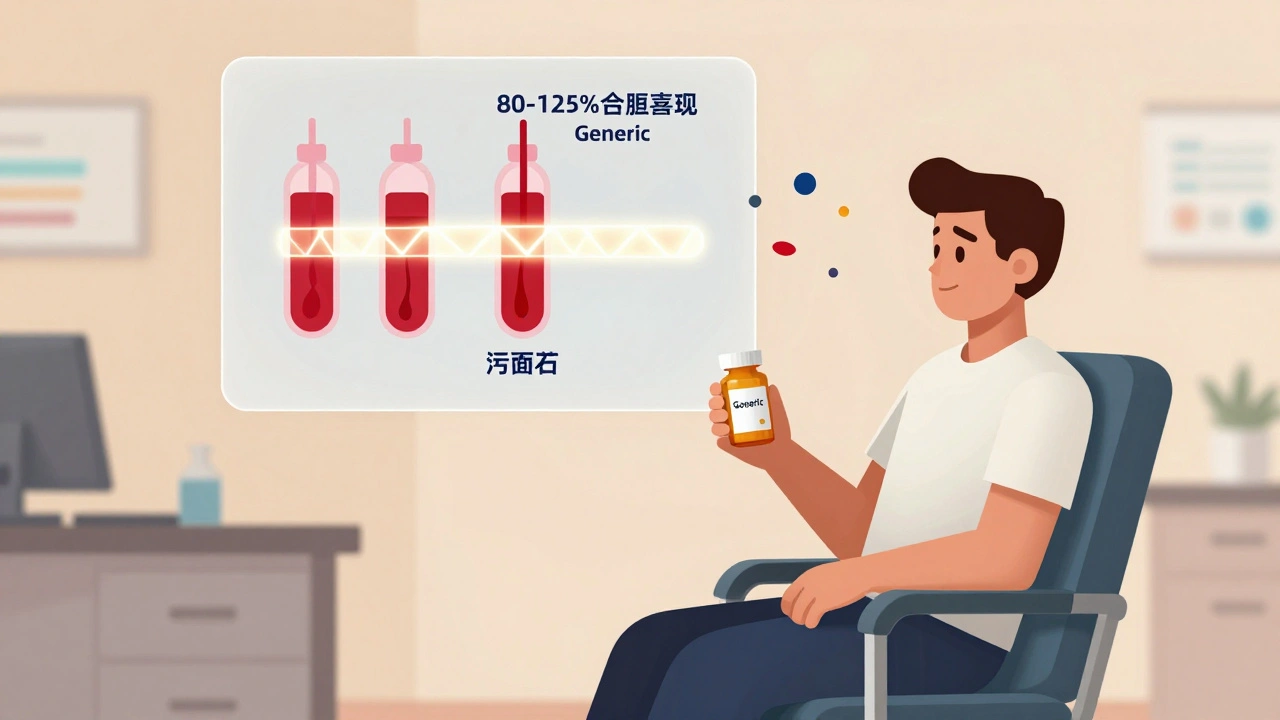
Most patients aren’t skeptical because they’re misinformed. They’re skeptical because they’ve been shown two pills that look nothing alike and told they’re the same. One is white, oval, and marked with a brand logo. The other is blue, round, and labeled with a pharmacy’s name. No wonder they think: "Is this really the same?" A 2023 study found that 63% of patient concerns about generics come down to appearance. Another 27% are about whether the generic works as well. And 10%? They’ve had a bad experience-maybe a headache after switching-and now they blame the pill, not the change in inactive ingredients like dyes or fillers. The truth? The FDA requires generics to deliver the same amount of active ingredient into the bloodstream as the brand-name version, within a 90% confidence interval of 80-125%. That’s not a guess. That’s science. For every 100 patients who take a generic blood pressure pill, 98 will get the exact same therapeutic result as if they took the brand. But if you don’t say that out loud, patients fill the silence with fear.What Makes a Generic a Generic?
Let’s clear up the confusion. A generic drug must meet these exact standards:- Same active ingredient (the part that treats the condition)
- Same strength and dosage form (tablet, capsule, liquid)
- Same route of administration (oral, injectable, etc.)
- Same bioequivalence (absorbed into the body at the same rate and amount)
- Same manufacturing quality standards (same inspections, same testing)
The Real Cost Difference
Here’s what matters most to patients: money. Generic drugs cost 80-85% less than brand-name versions. For someone on Medicare or with a high-deductible plan, that’s not a savings-it’s survival. Take rosuvastatin. The brand-name Crestor can cost $300 a month. The generic? Around $10. A patient switching from brand to generic can save $3,000 a year. That’s a rent payment. A grocery bill. A bus pass to get to their next appointment. In 2022, U.S. patients saved $373 billion using generics. Medicare Part D enrollees saved an average of $1,269 per year. These aren’t numbers on a chart. They’re real people choosing between pills and food. But here’s the catch: if a patient stops taking their medication because they think the generic doesn’t work, the cost skyrockets. Emergency visits. Hospital stays. Missed work. That’s the hidden price of poor communication.How to Talk About Generics-The TELL Method
You don’t need a 20-minute lecture. You need five minutes. And you need to listen first. The American Pharmacists Association recommends the TELL framework:- Tell: "This generic has the same active ingredient as your brand-name pill. It’s not a different medicine-it’s the same treatment, just less expensive."
- Explain: "The color and shape changed because of trademark rules. The ingredients that help it work are identical. The ones that don’t-like dyes-are different, but they’re safe."
- Listen: Don’t assume they’re worried about cost. Ask: "What are your concerns about this change?" Maybe they had a bad reaction last time. Maybe their cousin said it didn’t work. Listen. Don’t interrupt.
- Link: "This change means you can afford to take it every day. That’s how we keep your blood pressure under control and avoid a stroke down the road."
What to Say When They Say, "It Doesn’t Work Like Before"
Patients don’t say, "I’m worried about bioequivalence." They say, "This one doesn’t work as well." Here’s how to respond:- If they mention a change in side effects: "Sometimes, when we switch to a new formulation, your body needs a few days to adjust. If you notice anything unusual-like dizziness or nausea-let us know. But it’s not because the medicine is weaker. It’s because the fillers changed."
- If they say, "I used to feel better on the brand": "That’s common. But studies show that for most people, the effect is the same. In fact, 47 studies involving over 9,000 patients found no difference in effectiveness between generics and brands for heart medications."
- If they’re still unsure: "We can try the brand again, or we can try a different generic manufacturer. Some people respond better to one version than another. Let’s find what works for you."
When to Be Extra Careful
Not all drugs are created equal when it comes to switching. For medications with a narrow therapeutic index-where even small changes in blood levels can cause problems-you need to be more cautious. Examples:- Levothyroxine (for thyroid)
- Warfarin (for blood thinning)
- Phenytoin (for seizures)
- Cyclosporine (for organ transplants)
What Works: Real Stories From the Front Lines
A 68-year-old woman in Melbourne came in upset because her new generic metformin was a different color. She’d been on the brand for years. She thought the change meant her diabetes was getting worse. Her pharmacist didn’t just explain the science. He showed her the FDA’s website on generics. He told her, "This pill has the same active ingredient as your old one. The only difference is the color. But the price? It’s $250 less a year. That’s $20 a month you can use for groceries or bus fare." She left with a printed fact sheet. Three months later, she came back smiling. "I’ve been taking it every day. I didn’t realize how much I was stressing over the color." Another patient, a 52-year-old man on a fixed income, refused his generic atorvastatin because he’d read online that generics were "made in China" and "unsafe." His pharmacist didn’t argue. He said, "Let me show you how the FDA inspects every factory-even in China-that makes medicine sold in the U.S." He pulled up a video from the FDA showing inspectors checking production lines. The patient watched. Then he said, "Okay. I’ll try it." He’s still on it. Two years later.
What Doesn’t Work
Saying: "It’s the same thing." That’s not enough. Patients hear that and think: "You’re just trying to save money." Saying: "Your insurance made me switch." That shifts blame. Patients feel powerless. Saying: "Everyone takes generics." That’s not reassuring. It’s dismissive. The goal isn’t to convince. It’s to connect.Tools That Help
You don’t have to wing it. Use these:- Teach-back method: After explaining, ask: "Can you tell me in your own words why this generic is safe?" This boosts retention by 40%.
- Printed handouts: The FDA and APhA offer free, plain-language fact sheets in multiple languages.
- Video explainers: New FDA-funded videos (2023) show real patients explaining their switch. Use them in waiting rooms.
- Documentation: Note in the chart: "Patient counseled on generic substitution. Concerns: appearance. Addressed with FDA info sheet. Patient agreed to trial."
The Bigger Picture
Generics aren’t just about cost. They’re about access. About dignity. About letting someone take their medicine every day without choosing between pills and rent. In 2022, 90% of all prescriptions filled in the U.S. were generics. That’s up from 19% in 1984. That’s not a fluke. It’s policy. It’s science. It’s progress. But progress doesn’t mean anything if patients don’t take the pills. Your job isn’t to sell generics. It’s to make sure the right person gets the right medicine-every day. And sometimes, that means turning a $300 question into a $10 answer.What’s Coming Next
Biosimilars-complex generics for biologic drugs like insulin and rheumatoid arthritis treatments-are starting to hit the market. The FDA has approved 43 so far. These are harder to explain. They’re not exact copies. They’re highly similar. The communication challenge is bigger. But the same rules apply: listen first. Explain clearly. Link to the patient’s life. The future of healthcare isn’t just cheaper drugs. It’s better conversations.Are generic medications really as effective as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and bioequivalence as the brand-name version. This means they deliver the same amount of medicine into the bloodstream at the same rate. Over 47 studies involving more than 9,000 patients found no meaningful difference in effectiveness for heart medications, antidepressants, and other common drugs. The only differences are in inactive ingredients like color or shape, which don’t affect how the drug works.
Why do generic pills look different from brand-name ones?
Trademark laws prevent generic manufacturers from making pills that look exactly like brand-name versions. That’s why the color, shape, or marking might be different. But the active ingredient-the part that treats your condition-is identical. These visual changes are purely for legal reasons, not because the medicine is different.
Can switching to a generic cause side effects?
Rarely. Side effects are usually caused by the active ingredient, which doesn’t change. But sometimes, switching to a different generic (or even a different batch) can cause minor reactions due to changes in inactive ingredients like dyes or fillers. If you notice new symptoms after switching, talk to your provider. It’s not because the generic is weaker-it’s because your body might need a few days to adjust to a new formulation.
Are generics made in the same quality facilities as brand-name drugs?
Yes. The FDA inspects all manufacturing facilities-whether they make brand-name or generic drugs-using the same strict standards. Many brand-name companies even produce their own generics under different labels. The difference isn’t in the factory. It’s in the price.
What should I do if my patient refuses to take a generic?
Don’t push. Listen first. Ask what their concern is-cost, appearance, past experience? Use the TELL method: Tell them it’s the same medicine, Explain the visual differences, Listen to their worries, and Link the switch to their health goals. Offer a trial. Provide printed FDA materials. If they’re still unsure, consider switching to an authorized generic (made by the brand company) as a bridge. Most patients will accept generics once they understand why.


Deborah Jacobs
My grandma switched to generic metformin last year and thought she was getting a knockoff until I showed her the FDA page. Now she prints out the fact sheets and hands them to her friends at the senior center. She says, 'If it’s good enough for the feds, it’s good enough for me.' And she’s been stable for 14 months. No headaches. No crashes. Just cheaper pills and more peanut butter on her toast.
It’s not magic. It’s just science with a price tag.