Exclusivity Periods: How Drug Patents Block Generic Access
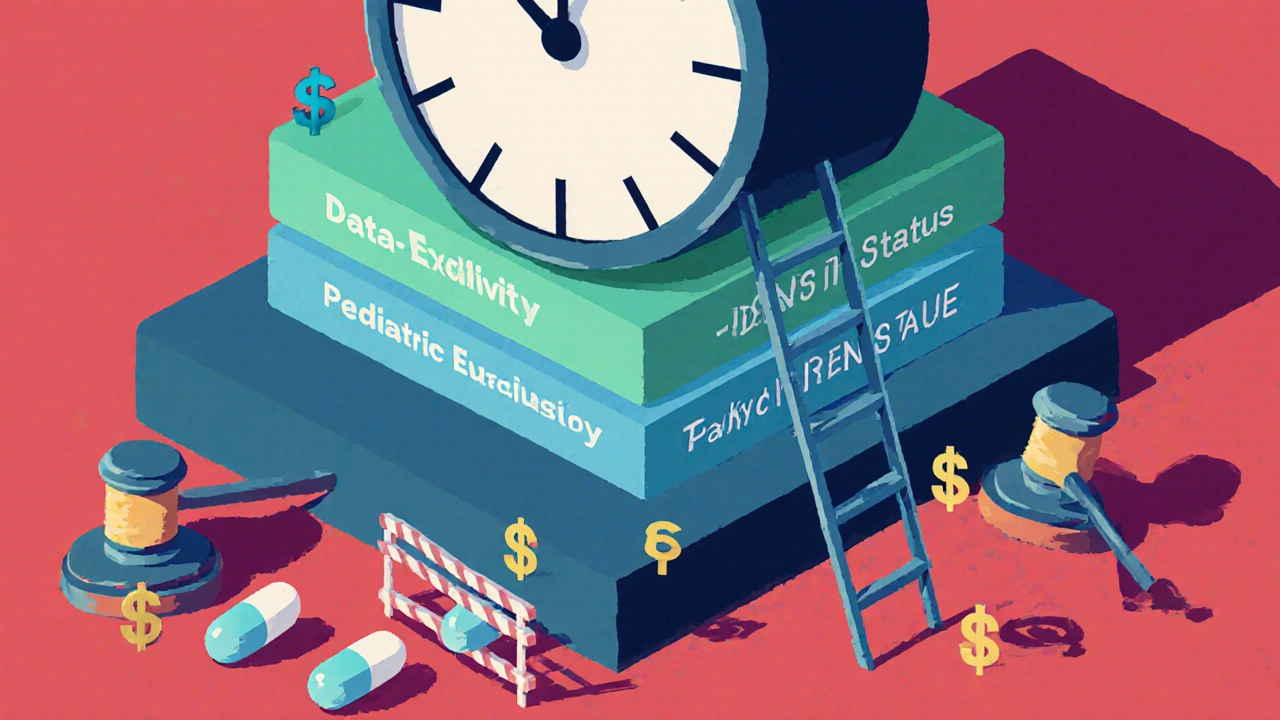
When a drug company gets approval for a new medicine, it doesn’t just get a patent—it gets an exclusivity period, a government-granted window where no other company can sell a generic version, even after the patent expires. This isn’t about innovation—it’s about control. These periods can last from 3 to 12 years, depending on the drug and the loophole used, and they’re the main reason why life-saving medications stay outrageously expensive long after the science is public. While patents protect inventions, exclusivity periods, a separate legal tool used by the FDA and other regulators to delay generic competition. Also known as market exclusivity, they’re often layered on top of patents to extend monopolies even further. You might think patents are enough, but companies use exclusivity to lock in profits without having to invent anything new.
How do they do it? One common trick is evergreening, making tiny changes to a drug—like switching from a pill to a liquid or adding a new coating—to qualify for a fresh exclusivity period. Another is pediatric exclusivity, a 6-month extension granted when a company tests a drug on children, even if the results don’t change how the drug is used. These aren’t loopholes by accident—they’re built into the system. The result? A single drug like Humira has had its exclusivity extended over 20 times, keeping generics off the market for more than two decades. Meanwhile, compulsory licensing, a legal tool that lets governments override patents during health emergencies, is rarely used in wealthy countries, even when drug prices kill people. Patients pay the price. A generic version of a drug might cost $5 a month, but during exclusivity, the brand version can run $500. That’s not just a markup—it’s a tax on illness.
And it’s not just about money. Exclusivity periods delay access for millions who need affordable treatment—whether it’s for diabetes, heart disease, or mental health. Doctors want to prescribe generics, but they can’t if they don’t exist. Medical schools teach bioequivalence, but patients still get stuck with expensive brands because the system rewards it. The posts below dig into how this plays out in real life: how companies stretch exclusivity with minor tweaks, how governments fight back, how patients suffer, and how some providers are finally pushing for change. You’ll see the tactics used to keep prices high, the legal tools that could break them, and the real human cost of delaying generics. This isn’t theory. It’s happening right now, in your pharmacy, in your wallet, in your health.
Generic drug exclusivity periods vary widely by country, affecting how quickly affordable versions become available. Learn how the U.S., EU, Canada, Japan, and others protect brand drugs - and who pays the price.
Continue reading...