MDR‑TB Alternatives: Effective Options Beyond First‑Line Drugs
When dealing with MDR‑TB alternatives, treatments used when Mycobacterium tuberculosis resists standard medications. Also known as drug‑resistant TB options, they provide a lifeline for patients who cannot be cured with the usual rifampicin‑isoniazid combo.
Key Second‑Line Drugs You Should Know
The most talked‑about alternatives are Bedaquiline, a diarylquinoline that targets the ATP synthase of TB bacteria, Delamanid, a nitro‑imidazooxazole that blocks mycolic acid synthesis and Linezolid, an oxazolidinone effective against many resistant strains. Together they form the backbone of WHO‑recommended shorter regimens, cutting treatment time from 20‑24 months down to 9‑12 months in many cases.
Understanding why these drugs matter starts with the biology of resistance. Mycobacterium tuberculosis develops mutations that render rifampicin and isoniazid ineffective, leading to MDR‑TB. When the bacterium acquires additional changes, it can become extensively drug‑resistant (XDR‑TB), demanding even more potent alternatives. The presence of rifampicin resistance, a hallmark of MDR‑TB often signals the need for a full‑scale regimen shift.
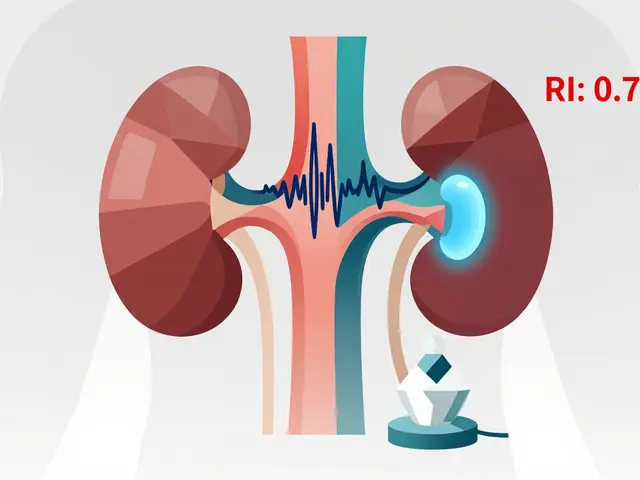
International guidelines now favor a combination of Bedaquiline, Delamanid, and Linezolid plus a fluoroquinolone, forming an "all‑oral" regimen that avoids injectable drugs. This approach reduces the risk of hearing loss and kidney damage associated with older treatments. The World Health Organization (WHO) and national TB programs have embraced these regimens because they improve cure rates and lower relapse risk.
Side‑effect management is a critical piece of the puzzle. Bedaquiline can cause QT‑interval prolongation, so baseline ECGs and regular monitoring are mandatory. Delamanid shares similar cardiac concerns, while Linezolid often leads to peripheral neuropathy and bone‑marrow suppression. Clinicians must balance efficacy with toxicity, adjusting doses or swapping agents when adverse events emerge.
Patient adherence remains the biggest hurdle in MDR‑TB care. Directly observed therapy (DOT) programs, community treatment supporters, and digital adherence technologies all help ensure that patients complete their lengthy courses. Studies show that supportive counseling and socioeconomic assistance boost success rates dramatically, turning a daunting regimen into a manageable daily routine.
Accurate diagnosis guides the choice of alternatives. Rapid molecular tests like GeneXpert detect rifampicin resistance in under two hours, while culture‑based drug‑susceptibility testing confirms the full resistance profile. These tools let doctors target the right combination of second‑line drugs from day one, shortening the period of ineffective therapy.
Research continues to expand the MDR‑TB toolbox. New drugs such as pretomanid, approved for a three‑drug combination with Bedaquiline and Linezolid, show promise for highly resistant cases. Clofazimine, originally an anti‑leprosy agent, is being repurposed for TB and adds another option for constructing individualized regimens.
Cost and access can still limit the reach of these lifesaving alternatives. Generic production of Bedaquiline and Delamanid has lowered prices in several regions, and international funding mechanisms help subsidize treatment for low‑income patients. Knowing where to find affordable sources can be the difference between cure and chronic illness.
Below you’ll find a curated collection of articles that dive deeper into each of these topics—drug comparisons, side‑effect management, patient‑support strategies, and the latest research breakthroughs. Use them to build a solid understanding of MDR‑TB alternatives and to choose the best path forward for yourself or your loved ones.
A detailed comparison of Trecator SC (Ethionamide) with other second‑line TB drugs, covering mechanisms, side effects, costs, and how to choose the right treatment.
Continue reading...