Amiloride: What it Does, How to Use It, and Safety Tips
If your doctor mentioned amiloride, you probably want the straight facts. Amiloride is a potassium-sparing diuretic often used for high blood pressure and to prevent potassium loss when other diuretics are needed. It helps the kidneys remove extra water without dumping potassium the way thiazides do.
How amiloride works and when people take it
Amiloride blocks specific channels in the kidney that let sodium pass into urine. With less sodium reabsorbed, the body excretes more water, lowering blood volume and blood pressure. Doctors prescribe it alone or together with a thiazide diuretic so the thiazide’s tendency to lower potassium is balanced by amiloride’s potassium-sparing effect.
Common reasons to use amiloride include managing hypertension, treating edema (swelling), and protecting potassium levels when on longer-term diuretics. It's also used by some patients with certain rare kidney-related conditions, but your clinician will decide if it fits your situation.
Practical tips: dosing, side effects, and interactions
Typical adult doses are low and start small — many people take a single daily tablet. Doctors adjust dose based on blood pressure, kidney function, and potassium levels. Don’t change dose on your own; small changes can affect potassium a lot.
Watch for the main side effect: high potassium (hyperkalemia). Symptoms can be subtle — weakness, tingling, or irregular heartbeat. Other common effects include dizziness, nausea, and headache. If you feel faint or notice a racing or skipped heartbeat, call your provider.
Important interactions to remember: combine amiloride with ACE inhibitors, ARBs, aldosterone blockers (like spironolactone), or potassium supplements and you raise the risk of dangerous high potassium. NSAIDs can blunt diuretics' effects and affect kidney function. Your doctor will likely check blood potassium and creatinine soon after starting or changing doses.
Special caution if you have reduced kidney function. If your kidneys aren’t clearing waste well, amiloride can push potassium too high. Elderly patients may need smaller doses and closer monitoring.
Practical checklist before starting amiloride: tell your prescriber about all medicines (including OTC potassium, herbal supplements, and NSAIDs), get a baseline potassium and kidney test, and schedule follow-up labs about a week or two after starting or changing dose.
Want more reading from this site? Check posts about blood pressure and diuretics like “Toprol: Benefits, Side Effects, and Alternatives for Heart Health” and “5 Alternatives in 2025 to Chlorthalidone” to compare options and learn how different drugs affect blood pressure and potassium.
If anything here sounds risky for you, talk to your doctor or pharmacist. They’ll personalize the plan — dose, monitoring, and whether amiloride is the right fit. Small drug choices matter, and a quick lab test can keep things safe.
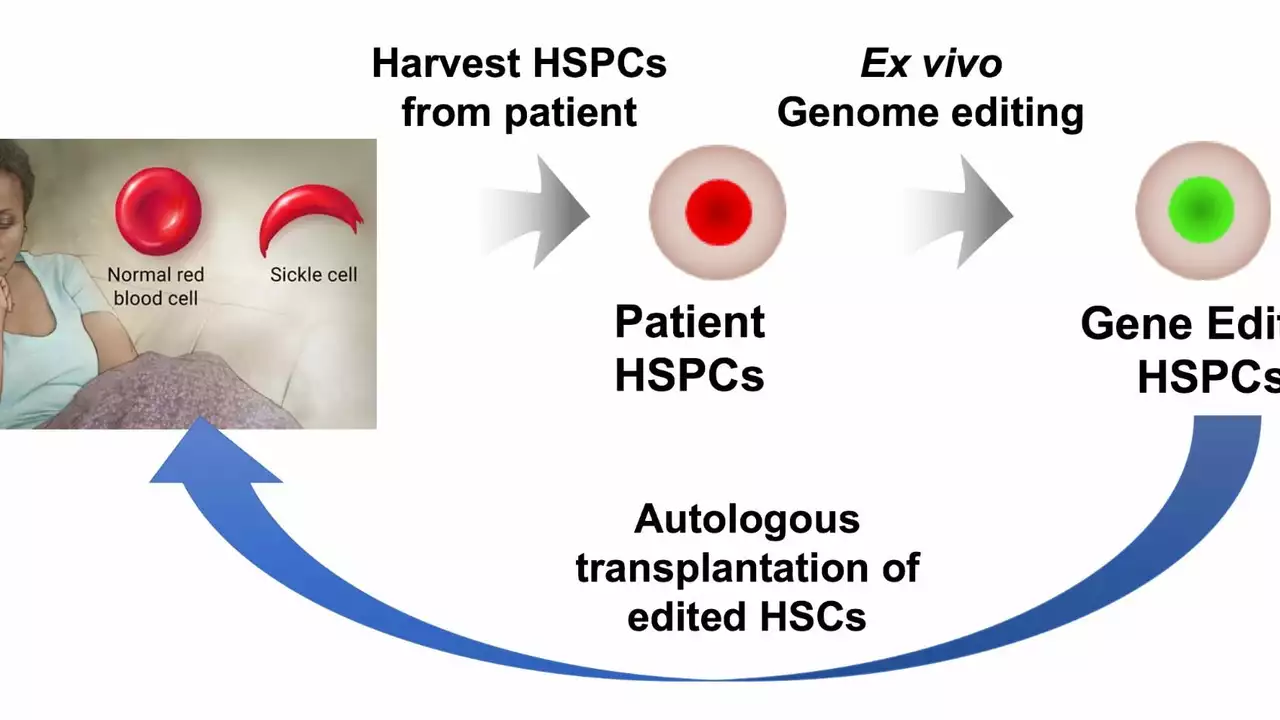
I recently came across some intriguing research on Amiloride and its potential role in treating Sickle Cell Disease. Amiloride is a medication primarily used to treat high blood pressure and heart failure. However, studies have suggested that it could also help reduce painful symptoms and complications associated with Sickle Cell Disease. This is mainly due to its ability to inhibit certain ion channels, reducing the sickling of red blood cells. The prospect of Amiloride as a treatment for Sickle Cell Disease is exciting, and I'm eager to see how further research develops in this area.
Continue reading...