Bioequivalence: What It Means for Generic Drugs and Your Health
When you pick up a generic pill, you’re not just saving money—you’re relying on something called bioequivalence, the scientific proof that a generic drug performs the same way in your body as the brand-name version. Also known as therapeutic equivalence, it’s the quiet guarantee that your cheaper medication won’t just look the same—it’ll act the same. This isn’t marketing. It’s chemistry, pharmacology, and strict testing rolled into one rule: if two drugs are bioequivalent, your body absorbs them at the same rate and to the same extent. No guesswork. No hidden differences.
That’s why generic drugs, medications approved by health agencies after proving they match brand-name drugs in performance are trusted worldwide. They don’t cut corners. They go through real studies—measuring blood levels, tracking how fast the drug enters your system, and checking how long it stays active. If the numbers fall within a tight range (usually 80% to 125% of the brand), it’s approved. That’s the standard for drug equivalence, the measurable outcome that ensures a generic delivers the same clinical result. It’s not about ingredients being identical—it’s about what they do inside you.
And it’s not just for pills. Bioequivalence applies to patches, inhalers, injections—even eye drops. That’s why a fentanyl patch from a generic maker works the same as the brand, as long as it meets the standard. That’s why your blood pressure pill, your antibiotic, or your antidepressant won’t suddenly stop working just because the label changed. The science behind it is solid. The FDA, EMA, and other global agencies don’t approve generics without proof. You’re not taking a risk—you’re using a validated alternative.
Some people worry that generics are "weaker" or "less reliable." But if a drug is labeled bioequivalent, that’s not true. The difference between a brand and its generic? Usually less than 5% in how your body handles it. That’s less variation than between two batches of the same brand-name drug made months apart. What changes is the price. And the packaging. And sometimes, the color of the pill. Not the effect.
What you’ll find here are real-world stories and clear breakdowns of how bioequivalence plays out in practice. From how heat affects fentanyl patches to why switching antibiotics like sulfamethoxazole still works, every post ties back to this simple truth: if it’s bioequivalent, it’s safe and effective. You’ll see comparisons of blood pressure pills, glaucoma drops, antidepressants, and emergency contraceptives—all grounded in the same science. No fluff. No jargon. Just what you need to know to trust your meds, save money, and stay in control of your health.
IVIVC lets pharmaceutical companies replace costly human bioequivalence trials with lab-based dissolution tests. When done correctly, it saves millions and speeds up generic drug approvals - but only a fraction of submissions succeed.
Continue reading...
Generic drugs save billions in healthcare costs and are just as effective as brand-name medications. This article explains the full manufacturing process - from reverse engineering to FDA approval - and why quality control is non-negotiable.
Continue reading...
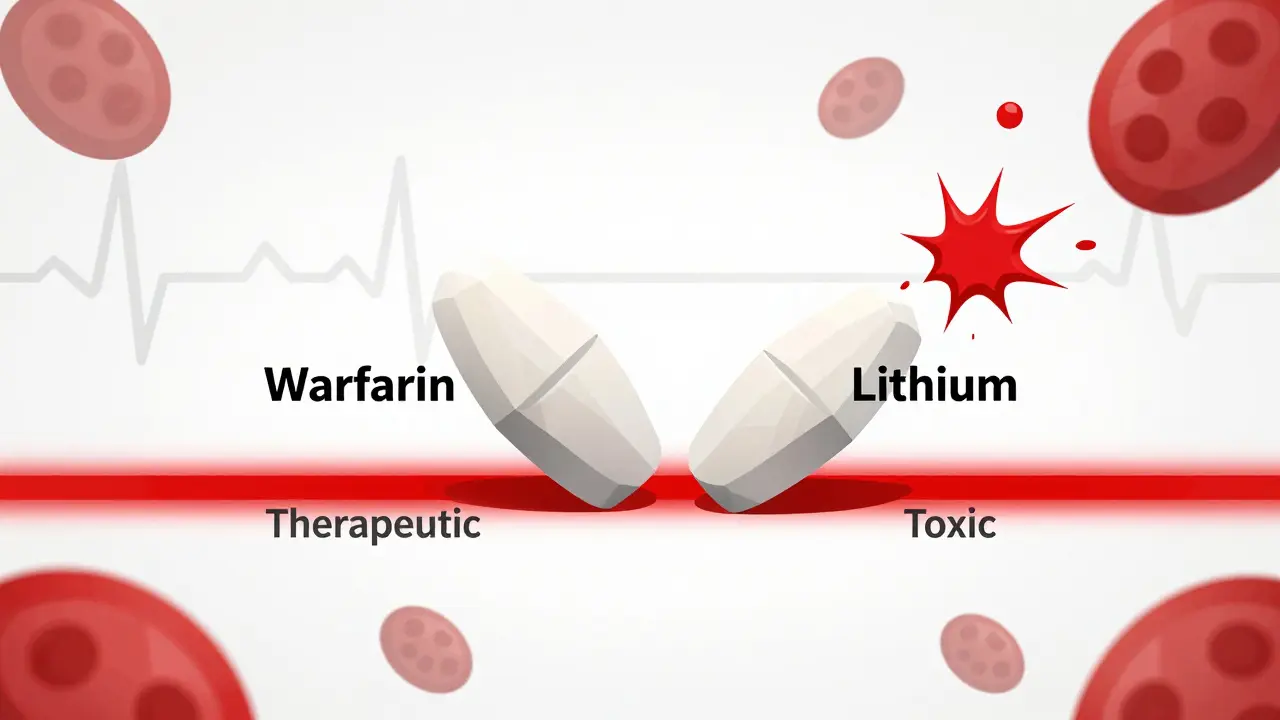
Combination NTI drugs offer powerful treatment for complex conditions but carry high risks when generics are substituted. With no approved generic combinations in the U.S., patients face safety gaps, high costs, and inconsistent care.
Continue reading...
Doctors prescribe generics for 90% of medications, but many still don't understand or trust their equivalence. This article explores why medical education fails to teach bioequivalence, how habits override science, and what changes can make generics the default - not the compromise.
Continue reading...