Brand Drugs: What They Are, Why They Cost More, and How Generics Compare
When you hear brand drugs, the original, patented versions of medications sold under a company’s trademark name. Also known as originator drugs, they’re the first version of a medicine to hit the market after years of research and clinical trials. These are the pills and patches you see advertised on TV — the ones with catchy names like Xyrem, Betoptic, or Tofranil. But behind every brand drug is a story of patents, profits, and price tags that often leave patients wondering: why is this so expensive?
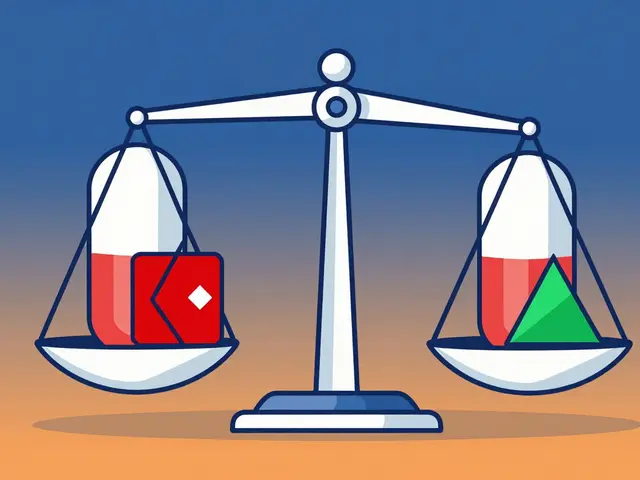
Patent exclusivity, a legal shield that lets drugmakers be the only ones to sell a drug for a set time. Also known as market exclusivity, it’s the reason you can’t buy a cheaper version right away. In the U.S., this can last up to 12 years for some drugs, thanks to extensions and loopholes like evergreening, when companies make tiny changes to a drug just to reset the patent clock. Also known as patent evergreening, it’s a strategy that keeps generics off shelves — and prices high. Meanwhile, generic drugs, the same medicine, same active ingredient, same effect, but sold without the brand name. Also known as non-brand medications, they’re often 80-90% cheaper once the patent expires. The FDA says they’re just as safe and effective. So why do doctors still prescribe brand drugs? Sometimes it’s habit. Sometimes it’s pressure from reps. And sometimes, patients just don’t know the difference.
What you’ll find in these articles isn’t just theory — it’s real talk from providers, patients, and policy experts. You’ll learn how brand drugs are protected by legal tools like compulsory licensing and Hatch-Waxman Act rules, how heat can turn a fentanyl patch into a danger zone, and why some doctors still don’t trust generics even when science says they’re identical. There’s no fluff here. Just clear answers about why your prescription costs what it does, how companies keep prices up, and what you can do to get the same results without paying extra.
Learn why generic drugs save up to 85% on prescriptions while matching brand effectiveness. Discover FDA standards, pricing trends, and how to save money on medications.
Continue reading...
Authorized generics are the exact same drug as brand-name medications, made by the same company with identical ingredients. Learn how they compare to regular generics and why they’re a trusted, lower-cost alternative.
Continue reading...
Doctors write 'Do Not Substitute' on prescriptions when brand-name drugs are medically necessary-especially for narrow therapeutic index drugs like levothyroxine or warfarin. Here’s why generics aren’t always safe, how often this happens, and what patients should know.
Continue reading...